P&T Journal, the most widely read pharmacy publication, has included meeting overviews and feature articles by Walter Alexander for 15 years. Click for a sampling of these pieces.
Author: planetlink
An Integrated Approach for Clinical Trial Patient Retention
Scott H. Connor, Vice President, Marketing, Acurian
 Recruiting the right patients in sufficient numbers to clinical trials is a well-recognized challenge. The growing and equally critical challenge is keeping them in the studies for their duration.
Recruiting the right patients in sufficient numbers to clinical trials is a well-recognized challenge. The growing and equally critical challenge is keeping them in the studies for their duration.
In Phase III trials a full 30% of patients drop out, said Suzanne Elvidge in her article “Importance of Patient- Retention Strategies,” (April 2010, Life Science Leader, citing a CenterWatch analysis). The overall rate might actually be quite worse, according to a study from the Tufts Center for the Study of Drug Development (KI Kaitin, “Growing Protocol Design Complexity Stresses Investigators, Volunteers,” Impact Report, 2008) on 57 Phase II and III protocols. The report showed that between assessments in 1999- 2002 and in 2003-2006 clinical trial retention rates fell from 69% to 48%. Such high dropout rates can endanger the statistical validity of the clinical trial data analyses and render the findings unacceptable to worldwide regulatory agencies. Attempting to rebuild a depleted patient cohort with replacements midstream may be prohibitively costly and logistically cumbersome. This makes having patient retention strategies in place proactively an essential ingredient for a successfully conducted clinical trial. Given the clearly growing challenges to ensuring patient retention and research data collection, the modest added program cost of building in such strategies may be easily justified. In fact, many clinical operations directors and trial managers regard patient retention services as an affordable insurance policy to protect against the more severe cost implications caused by lost patients.
Traditional retention programs, however, have done a poor job of establishing success metrics or gaining momentum with research sites because of the very nature of their design. The cottage industry emerging over the last decade focusing on the patient retention portion of the clinical trial equation has attacked the problem in a fragmentary, decentralized manner. The major emphasis has been to reward patient participation with modest gifts, a strategy that is void of tracking or metrics, not to mention scrutiny due to recent changes in industry ethics codes. Further, distribution and warehousing of gifts is often a burden to sites, and ongoing, two-way communications between patients and sites is non-existent in this traditional approach, yet is an important part of patient satisfaction and retention.
New World Order
Acurian (the company), an established leader in patient recruitment and retention, has recently introduced its Retention Manager™ software platform, an innovative, comprehensive program that combines communication software with an array of direct services in support of patient retention. After conducting primary market research with patients, sites and sponsors, the company realized that the patient-site relationship is key to retention, and study coordinators require more efficient methods for forging stronger communication bonds with patients.
Case study data from a well-known telecommunications company in the clinical research space supports the premise that communication technology, such as cell phone text messages, has a positive impact on retention rates. The company compared the retention effects of using text message-based study visit and compliance reminders in a phase II bipolar study, as compared to an identical bipolar study that did not use communication technology. The use of text messaging reduced patients
lost to follow up by 11% and early withdrawal by 9%. Acurian’s Retention Manager goes beyond simple text messaging to include additional technologies and services described later in this paper.
The Conventional Approach
For the past decade, much creativity has been directed towards finding ways to incentivize patients’ ongoing commitment to the clinical trial process. Patients are provided with informational booklets, invitations to join associations, various tchotchkes, thermoses, tote bags and t-shirts with an imprinted study logo, practical health-related aids to exercise or diet (eg, diabetes recipes and food guides), and assorted marketing give-aways—all designed to keep patients mentally engaged in the fact that they have made a commitment to the research project.
Typically, the research coordinator receives a large box packed with the brochures, stuffed animals, tote bags and pedometers, leaving the distribution to the site personnel, and more importantly the tracking of what is being done when to the site coordinator. At the same time, it is universal experience that site coordinators consider themselves to be overworked and ceaselessly “on the firing line.” And with the responsibility to be aware of where perhaps 20 or more patients are in a multi-stage protocol, and in larger centers, juggling multiple patient cohorts in multiple, disparate trials, it is easy to understand how the operant question may be: “Is this putting something else onto my plate or taking something off?”
The distribution of various study related gifts is common. Over 84% of more than 700 site coordinators surveyed said they have participated in studies offering giveaways of this nature (Patient Retention Services Assessment. MSP Analytics, Inc. December 2009). However, site coordinators assessed their value for keeping patients motivated positively toward participation in clinical trials as modest (3.1/5 as compared with 4.6/5 for expense reimbursement cards).
It is worth mentioning here the new ethics code of the Pharmaceutical Research and Manufacturers of America (PhRMA) unveiled in July 2008. Its ban on distribution of pens, mugs, pads or other similar items with drug names was unanimously endorsed by member companies, and prominent members (including Eli Lilly & Co., Johnson & Johnson, Pfizer Inc. and GlaxoSmithKline PLC) have issued statements of support. Though enforcement is voluntary, the code has had a chilling effect on distribution of promotional items and other perks throughout the medical community. The questionable value of such tactics for patient retention notwithstanding, this does underscore that in the current climate a stronger emphasis on direct personal and practical support of site managers and patients makes sense.
A further insight into patient motivation, afforded by a study (Clinical Trial Participation Insights, Survey Gizmo, April 2010, sponsored by Acurian) looking at patients who had participated in and remained in clinical trials, is that it was the altruistic aspect, the sense of contributing to the “greater good,” that played the strongest role in patients’ self-assessments of why they had remained enrolled throughout the clinical trial duration. Toward that greater good, the site coordinator’s core obligation lies in seeing that the patient’s portion of the research protocol is carried out. Patients have to make and keep appointments within the stipulated time windows, schedule and submit to lab tests or imaging as required, and stay with the trial throughout the follow-up period. Relentlessly keeping track of patients’ status with regard to all of this is complex and difficult, as is taking appropriate steps when patients miss or fall behind in their appointments. There are associated loose-leaf binders, file drawers and folders stuffed with paperwork, and temperamental software programs to be managed.
Early Warning Signs
Aside from worrying individual patients through the many details of the clinical trial process, the state of the overall data collection project has to be monitored closely. Is a pattern of missed or outside-the-window appointments emerging? Are patients dropping out at an excessive rate? How will the site coordinator identify the problem? Take appropriate corrective actions? Will the sponsor find out that a third of the patients have been lost four months after a problem emerges and at a point too late for reasonable strategic adjustments?
The fundamental insight embodied in the Retention Manager platform is that successfully orchestrating and managing the tasks and details necessary for fulfilling clinical trial protocols while retaining patients in them is an enormous undertaking. When site coordinators are called upon to accomplish the critical synthesis of gathering, communicating and acting on information, on assembling all of the essential pieces unassisted, all too often crucial steps simply get left out. Only a centralized, integrated and structured approach to workflow, one combining effective human services with well-designed software, will do the job.
Reduced Workload
What happens when a patient has not yet made an appointment for a physician visit required by the protocol? The company’s Retention Manager software shows the site coordinator which among the active patients currently eligible to be scheduled for an appointment have not yet made one and therefore need to be focused on urgently. It identifies the patient and, through a set of color-coded warnings, the number of days until the appointment window opens up and until it ends. It also notes if any laboratory testing is needed. Retention Manager generates a constant stream of communication within the system and between the patient and the site coordinator so that each knows what the next step is and what steps have already been taken. While the platform takes on 90% of the work of coordinating and structuring the sequence of tasks to be accomplished, the site coordinator retains the task of ensuring that a particular patient has an appointment within the visit window. The software and Acurian’s retention specialists take up the other tasks, such as informing the patient via calls or text messages about the appointment date, sending reminders about upcoming appointments, noting any requirements (e.g., no eating after midnight for tests), or when there are long intervals between visits, sending general encouragement notes to maintain patients’ interest in and engagement with the clinical trial. The overall upshot is that the site coordinator’s tasks are substantially reduced while simultaneously, general vigilance with respect to the trial’s state of affairs and awareness as to what tasks need to be completed in a particular timeframe are heightened.
This heightened level of communication enables busy study coordinators to maintain a positive bond with patients throughout the entire study, yet requires no significant additional work. The resulting effect is better retention.
Real-time, Actionable Metrics
The availability, at any point during the progress of the trial, of real-time snapshot reports (for example, on patient retention percentages or patient compliance with various aspects of the protocol such as making appointments or scheduling tests) helps site coordinators monitor the trial status and assures sponsors that the project is being competently managed.
When it becomes apparent that patients have not merely missed an appointment or two, but have lost interest and may be considering dropping out, Acurian’s retention specialists engage in an intensive recovery process with direct, respectful personal contacts. The first goal is to identify the underlying causes of patients’ dissatisfaction. Are they unhappy with their physicians? Are travel expenses excessive? Investigators can be switched. Additional travel reimbursement can be arranged. Every effort is made to quickly identify patients’ issues and to ameliorate their concerns and reconnect them with the clinical trial. When the potential effects of a patient dropping out on data analyses, regulatory review, and costs of recruiting and introducing replacements are taken into account, sponsors fully accept that such efforts/expenses are justified.
Instant Gratification
Further practical details such as providing patients with agreed upon reimbursement for travel expenses through the platform’s debit card module are handled seamlessly by the software. For the patient, instant reimbursement for study-related expenses means instant gratification, and validation that study compensation is delivered as advertised. Sites benefit greatly as well. Study coordinators can finally abandon cumbersome and risky payment methods such as live checks. The debit card approach simplifies and secures financial administration, which is typically not a core competency of research professionals. As a result, site staff can focus on enhancing patient care and customer service as part of the retention strategy, rather than handling complaints from patients regarding reimbursement delays or misplaced checks.
The Overall Effect
 What is accomplished through this combination of software and targeted communications? That which is usually a fragmented process, one that at key moments becomes unmanageable by virtue of the sheer volume of necessary tasks, is simplified, prioritized and coordinated—without adding to anyone’s workload, especially the study coordinator. Problems appear “on the radar” with sufficient leadtime for effective intervention so that all those patients who can possibly be reclaimed for the study are brought back in, avoiding compromise to data collection and excessive costs.
What is accomplished through this combination of software and targeted communications? That which is usually a fragmented process, one that at key moments becomes unmanageable by virtue of the sheer volume of necessary tasks, is simplified, prioritized and coordinated—without adding to anyone’s workload, especially the study coordinator. Problems appear “on the radar” with sufficient leadtime for effective intervention so that all those patients who can possibly be reclaimed for the study are brought back in, avoiding compromise to data collection and excessive costs.
A technology and services approach like Retention Manager has a bright future because of what appears to be a gloomy forecast for clinical study design. According to the previously referenced Tufts study, the overall duration of clinical trials has increased 74%, average case report forms have grown from 55 to 180 pages, and consent forms are getting longer and more complicated. Trial protocols have become more complex with higher average numbers of required procedures per protocol. In short, patients are being asked to do more over longer periods of time. This level of commitment must be supported by exceptional site service, vigilant twoway communication, appreciation and support, and instant reimbursement. Without this level of insurance policy in place, trial managers are risking their trial outcomes in an environment that is ultra competitive and unforgiving.
 About Acurian
About Acurian
Acurian is a leading full-service provider of clinical trial patient recruitment and retention solutions for the life sciences industry. Through its proprietary patient panel of over 65 million patients, centralized advertising capabilities, and a fully hosted enrollment management technology platform, Acurian is able to identify, contact, prescreen, and refer patients into clinical trials, all while supporting investigator sites with services to maximize the randomization potential of every referred patient. Since 1998, Acurian has supported over 400 protocols for more than 60 companies. Acurian’s investors include Euclid SR Partners, ProQuest Investments, JP Morgan Partners, Flatiron Partners, CDP Capital Technology Ventures, and Merck Capital Ventures.
For more information about Acurian, visit www.acurian.com
The last three 2013 issues (October-December) of the Journal of Clinical Hypertension, a conservative and traditional medical journal, each included a section of a major research review article on a topic that until relatively recently hard science, data-driven clinicians might not have taken seriously. The topic under consideration was replacing antihypertensive medications with appropriate nutrition and nutraceutical supplements.
In an interview, the author, Mark Houston, MD, commended the open-mindedness of the Journal of Clinical Hypertension editor, Michael A. Weber, MD, and commented that the article’s reception has been mostly highly positive. “People’s eyes have been opened,” he said, adding that there has been some amazement at how much science is in the literature to back up such strategies, and surprise as to the extent that hypertension patients are clamoring to know more about ways to avoid or reduce the polypharmacy that is being offered to them by conventional practitioners.
Dr. Houston is triple board certification. He is a Hypertension Specialist, board certified by the American Society of Hypertension (FASH) as well board certified in Internal Medicine (ABIM) and Anti-Aging Medicine (ABAARM). He also is a functional medicine practitioner, certified by the Institute for Functional Medicine( IFM). Following this certification he also completed two master of science degrees, one in nutrition and the other in metabolic medicine. He is an associate clinical professor of medicine at Vanderbilt University School of Medicine, director of the Hypertension Institute, Vascular Biology and Life Extension Institute and medical director of the Division of Human Nutrition at Saint Thomas Medical Group, Nashville TN.
Functional medicine practitioners, aware of the increase in complex, chronic disease such as diabetes, heart disease, hypertension, cancer, mental illness and autoimmune disorders, pilule focus on identifying the underlying causes of disease and look for interactions between genetic, environmental and lifestyle factors. They seek to promote health and vitality by integrating conventional practices with prevention through combinations of drugs and/or botanical medicines, supplements, therapeutic diets, detoxification, exercise and stress management rather than emphasizing acute symptom relief, urgent care and removal of illness and disease.
Hypertension
The most recent NHANES (National Health and Nutrition Examination Survey) figures for hypertension control rate for US-born adults, as of 2010, although improving, still hover below 50%. At the same time, millions of Americans have been turning to alternative and complementary therapies along with dietary supplements as substitutes or add-ons to conventional multi-drug pharmacologic therapy for hypertension, a variety of maladies, and general health support.
In his recent (February 2014) presentation at the Integrated Healthcare Symposium 2014 in New York City, Dr. Houston reaffirmed the paper’s message that a diet- and supplement-based strategy in combination with appropriate lifestyle change can sometimes but not always replace a pharmaceutical-based approach to treating hypertension and preventing target organ damage.
Definitions at odds
The Mayo Clinic’s website defines hypertension as “a common condition in which the force of the blood against your artery walls is high enough that it may eventually cause health problems, such as heart disease.” Dr. Houston reframes the issue, positing otherwise that hypertension is a “‘correct and chronic dysregulated vascular response with an exaggerated outcome of three finite responses ( inflammation, oxidative stress and vascular immune dysfunction) to the infinite insults to the blood vessel…” Those insults, both biomechanical and biohumoral (biochemical, metabolic and nutritional), lead to vascular damage, endothelial and vascular smooth muscle dysfunction with vasoconstriction and hypertension. The vascular system in this interplay with environmental-gene expression patterns is an innocent bystander, according to Dr. Houston. Elevated blood pressure is one among multiple responses to endothelial dysfunction and vascular smooth muscle dysfunction, both of which precede the development of hypertension by decades.
While recognizing the role of genetic predisposition, Dr. Houston emphasized the major role of environment. “Eighty percent of vascular disease is environmental. It is not genetic…so it’s important to tell this to your patients so they don’t feel that they are doomed to have a cardiovascular event if there’s a family history.” The key to prevention and treatment of hypertension and cardiovascular disease, then, is in modulation of the environmental insults and the downstream disturbances of gene expression patterns.
The two major players in vascular disease leading to hypertension are angiotensin II and nitric oxide. When chronically elevated, angiotensin II promotes excessive vasoconstriction and hypertension, inflammation, oxidative stress, vascular immune dysfunction, thrombosis and growth. It is also pro-atherogenic. Nitric oxide, its antithesis, causes vasodilation, is anti-hypertensive and anti-inflammatory, and it reduces oxidative stress, vascular immune dysfunction, and thrombosis. It is anti-atherogenic. Therapeutic strategies, through either pharmacologic agents or nutrients, would therefore aim at increasing nitric oxide availability and at decreasing the effects of angiotensin II.
As to the question “Which occurs first, the vascular disease or the hypertension?” most people now believe that the microvascular disease and the endothelial dysfunction occur first, Dr. Houston said, with the blood pressure as a marker. But once the blood pressure goes up, it causes more endothelial dysfunction. It is clearly then bi-directional, so both have to be treated at the same time in an integrative approach that improves vascular health, optimizes vascular biological function and structure, slows vascular aging and subsequent cardiovascular disease.
Pathophysiology
The components of hypertension’s pathophysiology include oxidative stress, inflammation and autoimmune dysfunction. Reactive oxygen and nitrogen species levels become higher in the arteries and kidneys, while oxidative defenses are decreased.
Inflammation is increased in the vasculature and kidneys through greater levels of high sensitivity C-reactive protein (Hs-CRP), leukocytosis, increased neutrophils and reduced lymphocytes. In the kidney, renin-angiotensin-aldosterone system activity is heightened. Also in the arteries and kidneys, autoimmune destruction is attended by increased white blood cells and involvement of T-helper cells and cytotoxic T-cells (CD4+/CD 8+). “If you couple this with genetics, epigenetics and environmental-genomic interactions, then you have the inflammatory fire, the volcano in your arteries and your heart ready to erupt at any time.”
Hs-CRP is both a risk marker and risk factor for hypertension and cardiovascular disease. The angiotensin type 1 (AT1) receptor when stimulated is known to be inflammatory and to increase oxidative stress, vascular immune dysfunction and hypertension. It is counterbalanced by the angiotensin type 2 receptor (AT2R). Hs-CRP inhibits endothelial nitric oxide synthase and reduces nitric oxide, downregulating the AT2R.
The induced vascular immune dysfunction feeds the same cycle, with vascular injury attracting monocytes, macrophages and CD4+ T lymphocytes, leading to release of pro-inflammatory mediators, TNF alpha, interferon and interleukins (especially IL-17), building on the cascade of angiotensin II-based hypertension genesis events.
It is only recently been recognized, Dr. Houston pointed out, that aldosterone is an immune stimulant. Angiotensin II can induce hyperaldosteronism, and more than 30 inflammatory genes are produced just through the effects of aldosterone. Blockade of aldosterone, even with persisting hypertension or in normotensive patients, reduces cardiovascular risk.
Considering genetics and epigenetics, Dr. Houston noted that most of the single-nucleotide polymorphisms (SNPs) related to hypertension and cardiovascular disease are associated with oxidative stress, inflammation and immune dysfunction. An analysis of a micro-array of genetic polymorphisms in hypertension showed most of them (31/49) to be upregulated to an inflammatory process. Coronary disease, as well, is correlated with inflammatory upregulation, more so than with what are considered to be the top five coronary disease risk factors (hypertension, dyslipidemia, hyperglycemia, smoking and obesity).
The new treatment approach, Dr. Houston said, views hypertension as a disease in which the vascular biology is altered and the arteries need to be treated appropriately through non-pharmacologic mechanisms: nutrition, nutraceutical supplements, antioxidants, weight loss and exercise, meditation and sleep. Then the pharmacologic approach can be integrated to get the maximum reduction and protection of the cardiovascular system. The preferred drugs are ACEIs, ARBs and calcium channel blockers. Dr. Houston, in general, does not recommend beta-blockers, diuretics, central alpha agonists or alpha blockers. “But if you change the lifestyle and give it some time, eventually you probably can get them off many of the drugs.”
The Joint National Commission guidelines, Dr. Houston noted, have provided a non-mechanistic, non-personalized approach to treating hypertension, such that the same strategy is applied generally to all patients. About a decade back, Dr. Houston and colleagues began stratifying patients according to plasma renin activity (PRA) (as advocated by John Laragh, MD, for about half a century) and aldosterone levels. Plasma renin is the enzyme that leads to angiotensin II. Those with elevated angiotensin II levels generally have elevated PRA. High renin hypertension (PRA >0.65 ng/ml/hr [about 70% of patients]) is associated with decreased intravascular volume and higher risk for MI, ischemic heart disease, stroke, congestive heart failure, chronic kidney disease, and cardiovascular and overall mortality. Renin drugs and nutraceuticals (ACEIs, ARBS, direct renin inhibitors, beta blockers and central alpha agonists) are recommended for this population. Low renin hypertension (PRA<0.65 ng/ml/hr [about 30% of patients]), associated with increased intravascular volume, is treated with volume drugs and neutraceuticals (calcium channel blockers, diuretics, serum aldosterone receptor antagonists like spironolactone and eplerenone and alpha blockers).
Diagnosis
Standard blood pressure measurements, because they often do not accurately reflect cardiovascular health, can be misleading and are likely to become obsolete, Dr. Houston said. The ability to non-invasively measure blood pressure in central arteries is an important advance because the central and brachial pressures do not always correlate. For example, Dr. Houston said, while the blood pressure measured brachially in a sitting patient receiving a beta blocker may be normal (120/80 mmHg) patient, the central pressure can be as much as 10 mmHg higher, with the patient remaining at significant risk, as demonstrated in the CAFÉ trial (The Conduit Artery Functional Endpoint Study).
But measuring central pressure still gives only one point in time. The new standard, however, is 24-hour ambulatory blood pressure monitoring (ABPM) that simultaneously measures the brachial pressure and the central pressure in the aorta. While it is standard of care in the UK, but not in the US, coding “white coat” or “labile” or occasionally “resistant” hypertension will elicit insurance approvals, Dr. Houston noted.
Twenty-four hour ABPM is superior to home and office blood pressure monitoring for predicting future cardiovascular events and target organ damage. It has been shown to reduce by 25% the number of patients needing drug therapy, and overall it has been shown to be cost effective.
Twenty-four hour ABPM reveals important parameters missed by brachial readings, including dipping status, nocturnal blood pressure, white coat and masked hypertension, circadian rhythms with the early morning surges known to be associated with cardiovascular events and strokes, load (the percentage of reading >140/90 mmHg), blood pressure highs, lows and variability. Nocturnal blood pressure predicts event risk much better than daytime pressures.
In healthy normotensive individuals, nocturnal blood pressure reductions are 27/15 mmHg lower than daytime readings. Cardiovascular risk is higher with over- and under-dipping by more than 10%. Excessive dipping (>20%) increases ischemic stroke risk and reverse dipping (0-20%) increase hemorrhagic stroke risk.
Non-dipping does not allow renal sodium excretion and is most common in sodium sensitive patients and African Americans. It is more likely to be found, as well, in patients with renal insufficiency, those with secondary forms of hypertension, diabetes, cerebral volume loss and cognitive impairment, left ventricular hypertrophy, refractory hypertension, obstructive sleep apnea and autonomic dysfunction. Non-dipping is highly correlated with coronary heart disease, cardiovascular disease, congestive heart failure, chronic renal failure, increased carotid intima media thickness, multifocal leukoencephalopathy and silent cerebral infarctions.
Treatment
Event rates are strongly affected by timing of administration; they are 25-50% lower when a drug is given at night. Also, most drugs may partially convert non-dippers to dippers if dosed nocturnally. The drugs that will not convert non-dippers are those recommended, Dr. Houston emphasized, by JNC (Joint National Committee) 1-8: thiazide diuretics (hydrochlorothiazide), thiazide-like diuretics (chlorthalidone) and the older beta-blockers like metoprolol and the other “ols.” The ones that will convert non-dippers are the angiotensin converting enzyme inhibitors (ACEIs), the angiotensin receptor blockers (ARBs) and most of the calcium channel blockers and perhaps one or two of the newer beta-blockers (nebevilol and carvedilol).
Dr. Houston noted that he is aware of only one supplement that has been studied that will convert non-dippers to a dipping status, and that is melatonin at nocturnal doses of 3-4 mg at night.
Nocturnal hypertension
Nocturnal hypertension, defined as night time blood pressure >120/70 mmHg, is more common than non-dipping and is found in about 70% of hypertensive patients. It is a more powerful predictor of cardiovascular morbidity and mortality than circadian, mean or daytime blood pressure. Among patients with nocturnal hypertension, dosing at night with a dipping status-converting drug (ACEI, ARB, calcium channel blocker, nebivolol) reduces events by 29-38%.
The same JNC-recommended hydrochlorothiazide and older beta-blockers are less effective at reducing central blood pressure. The CAFÉ study indicated that these agents may reduce brachial pressure while leaving centrally measured systolic blood pressure unchanged or higher (4.3 mmHg higher). At the same time, central aortic pulse pressure was 3.0 mg higher (on account of pulse wave augmentation). Central blood pressure is more predictive than brachial pressure with respect to cardiovascular disease, cardiovascular disease mortality, all-cause mortality and left ventricular dysfunction.
Returning to diuretics, Dr. Houston said that beyond failing to reduce central arterial pressure or to improve vascular function or microvascular structure, vascular remodeling or hypertrophy, compared to ACEIs, ARBs and calcium channel blockers they do not optimally reduce coronary heart disease (CHD) or myocardial infarction (MI). The reductions in stroke and myocardial infarction (MI) are 25% lower. JNC 8 still lists diuretics as Step I therapy. “I’m not sure why we are still recommending thiazide diuretics or older beta-blockers for hypertension with the amount of contrary data that has been published in major hypertension journals all over the world.”
If a diuretic is needed, among the comparative benefits with indapamide are better blood pressure control, 50% less hypokalemia, minimal to no hyperglycemia or insulin resistance, lipid neutrality, less microalbuminuria, renal benefits, and better cardiac effects. Chlorthalidone, would be an alternative to HCTZ with better CV outcomes and has longer duration of action, but is not as good as indapamide related to all the other metabolic effects and CVD outcome data, Dr. Houston said.
Similarly, rates of adverse effects are high with first and second generation beta-blockers, and refill and compliance rates are low. More favorable brachial and central blood pressure, augmentation index, pulse wave velocity, endothelial dysfunction, systemic vascular resistance, nitric oxide, antioxidant and other vascular and metabolic effects make nebivolol and carvedilol preferable.
“The only time I use beta- blockers now is in the post-myocardial infarction patient, the patient who has congestive heart failure (either systolic or diastolic) or who has an arrhythmia–like supraventricular tachycardia or premature ventricular contractions. In hypertension, beta-blockers are less effective in reducing central BP, CHD, MI and overall CV mortality compared to ACEI, ARB, CCB or these in combination, and they really make you feel bad,” Dr. Houston commented.
The best drugs
Calcium channel blockers are very good for reducing blood pressure and for reducing strokes at the same blood pressure level compared to any other class (by 10% more).
In combination,
Skipped a lot-laragh at 1:05
Nutrient Testing
By looking at nutritional correlations to vascular disease and hypertension and by performing a nutritional analysis on specific patients, a program that replaces nutritional deficiencies with vitamins, antioxidants, minerals and nutraceutical supplements can be initiated.
Every patient who comes to Dr. Houston’s office gets an intracellular lymphocyte analysis, a 6-month functional assay of a patient’s nutrients. It reveals what that lymphocyte is deficient in, and how much replacement would be required to make it work better. The most accurate assay, Dr. Houston said, is available only through SpectraCell Laboratories (Houston, TX), and is covered by some insurance plans. Typically many patients become normotensive by counterbalancing their nutritional and supplement deficiencies within 3 to 6 months.
The Hypertension Institute engages a full-time licensed nutritionist/exercise physiologist/personal trainer who sees and advises all of the patients. Information on relaxation and stress-reducing meditation is also provided. “It’s an extremely important part of what we do in cardiovascular medicine,” Dr. Houston remarked.
The recommended diet is essentially a Mediterranean diet with some modification: a lot of vegetables, some fruit, minimal to no carbohydrates, high quality organic protein, the right types of fats (primarily omega-3 fatty acids, monounsaturated fats, limited saturated fats and no trans fats).
Many of the natural compounds in food, as well as certain nutraceutical supplements, vitamins, antioxidants, or minerals mimic drugs, functioning in a similar fashion to a specific class of antihypertensive drugs. The potency, however, may be less, and they may take longer to work than the antihypertensive drug. When used in combination with other nutrients and nutraceutical supplements, though, the antihypertensive effect can be magnified.
Diuretics
Among the natural diuretics, vitamin B-6, taurine and magnesium are quite inexpensive and they work well together.
Beta blockers and central alpha agonists
Among the best are taurine and vitamin B-6 followed by potassium.
Direct vasodilators
Omega-3 fatty acids, magnesium and coenzyme Q-10 are among the best natural direct vasodilators. Dr. Houston commented that he has found the studies refuting the value of omega-3 fatty acids to be deeply flawed.
Calcium Channel Blockers
Among those with optimal activity are alpha lipoic acid, magnesium and omega-3 fatty acids (EPA + DHA).
Angiotensin converting enzyme inhibitors (ACEI)
Among the best natural ACEIs that has been studied is the dried bonito fish, which is in the tuna and mackerel family. Pycnogenol, the omega-3 fatty acids and hydrolyzed whey protein (which can also help with glutathione levels) are also effective.
Angiotensin receptor blockers (ARBs)
Testing the theory
Dr. Houston tested the strategy of repleting deficient nutrients in a 2010 study including 671 hypertensive patients with baseline off-medication blood pressures ranging from 140/90 mmHg to 210/115 mmHg. The objective was to assess the role of cellular micronutrients, nutraceuticals, vitamins, antioxidants and minerals in the prevention and treatment of hypertension and cardiovascular disease. Assays of micronutrient, plasma renin and aldosterone levels were performed. Treatment consisted of a comprehensive program including antihypertensive drugs, repletion of nutritional deficiencies, and therapeutic doses of appropriate nutritional supplements. Patients were put on a DASH 2 diet (fruits and vegetables, low sodium, high potassium, high magnesium, high fiber), and worked with a coach advising on exercise (aerobic and resistance exercises), meditation, and sleep.
Analysis revealed that hypertensive patients had significantly more micronutrient deficiencies compared to normotensive patients (n=2667) (p<0.0017), including biotin, serine, asparagine, calcium and vitamin D (p<0.0017), vitamin B1, choline, insulin, magnesium, Co!-10, lipoic acid, and total antioxidant level oxidative defense (p<0.05). After 6 months, antioxidant levels were improved significantly by 8.47% (p=0.03) and micronutrients were completely repleted in 97% of patients.
Over 6 months (range 4-12 months), 62% of the hypertensive patients were able to completely taper and/or discontinue anti-hypertensive drugs, reducing and maintaining their blood pressures to between 120/80 mmHg and 126/84 mmHg.
Dr. Houston underscored the economic implications, given the US year yearly expenditure on anti-hypertensive agents of about $20 billion per year (representing about 10% of the national drug expenditure). This program, he said, could lower drug costs by about $12.4 billion annually.
“That would get the attention of an insurance company, eventually,” he commented.
Combination therapy
Nutrients can be added to each other or to drugs to achieve additive or even synergistic benefits, not just on blood pressure, but also on vascular health and endothelial dysfunction. For example, sesame can be taken with beta blockers, diuretics with nifedipine; pycnogenol or R lipoic acid with ACE inhibitors; lycopene with various antihypertensive agents; vitamin C with a calcium channel blocker; NAC (N-acetylcysteine) with arginine. Other productive combinations include garlic with ACE inhibitors or diuretics or calcium channel blockers, and melatonin with an ARB.
Drug nutrient interactions
Dr. Houston cautioned that practitioners need to be aware of possible nutrient deficiencies caused by administration of antihypertensive drugs. Hydrochlorothiazide and chlorthalidone decrease potassium, magnesium, phosphorus, sodium, chloride, folate, B6, zinc, iodine and CoQ-10, while increasing homocysteine, calcium, creatinine, glucose, insulin resistance, type 2 diabetes mellitus at a rate of 5% per year, and the incidence of renal insufficiency at year 10 by more than 35%. First and second generation beta blockers lower CoQ-10 and ACE inhibitors and ARBs decrease zinc. “So check them and replete them,” Dr. Houston said.
Caution
Dr. Houston cautioned that the role of supplements in hypertension has not yet been tested in clinical outcome trials in the manner that conventional drugs have been assessed. So while there is an apparent role for supplements in treating hypertension, their ability to improve cardiovascular outcomes remains to be proven.
Further training note
Short of following Dr. Houston’s path of getting advanced degrees in nutrition and metabolic medicine, courses are readily available from among others the Institute of Functional Medicine and the American Academy of Anti-Aging Medicine.
Dr. Houston’s take home: “Hypertension can be treated from a more pathophysiological point of view by looking at inflammation, oxidative stress and vascular immune dysfunction. If you recognize those entities along with nutritional deficiencies and plasma renin activity and treat accordingly, many patients can have hypertension prevented or controlled without pharmacotherapy.”
Magnetic resonance imaging (MRI), physician the gold standard of soft tissue imaging, is being used more frequently and in more innovative ways. However, patients with implantable devices are generally ineligible for an MRI. Industry is working to solve the problem and develop MR conditional devices. Experts were questioned at the International Neuromodulation Society (INS) 11th World Congress in Berlin, Germany, June 8-13, 2013, about the status of neurostimulation devices and MRIs.
MRI is being used for a wide array of procedures – from cerebral glioma to MRI-guided gene therapy for brain cancer, heart catheterization, and pericardiocentesis – because it is non invasive and may be more precise than other imaging techniques such as x-rays and computerized tomography (CT) scans, which emit ionizing radiation that accumulates in the body. CT is well-suited for evaluating moderate-to-severe closed head injuries, suspected lung cancer, spine trauma, and suspected appendicitis.
For soft tissue assessment, however, the non-ionizing radiofrequency (RF) signal of MRI is often better suited. For example, in situations in which stroke, seizure, liver lesions, complicated low back pain, or acute joint trauma are known or suspected, MRI would be the preferred choice if safety could be guaranteed, according to MRI safety expert Gregor Schaefers, managing director of MR:comp in Gelsenkirchen, Germany, at a Medtronicsponsored INS symposium.
Lars Jönsson, MD, a neuroradiologist from Sahlgrenska University Hospital in Göteborg, Sweden, speaking at that Medtronic symposium, emphasized that MRI offers the best imaging in many anatomical areas and the only good imaging in some others. MRI also helps patients avoid risky or painful exams, treatment such as myelography, arthroscopy, and endoscopic retrograde cholangiopancreatography (ERCP).
The use of implantable devices – from cardiac pacemakers and implantable cardioverter defibrillators (ICDs) to neurostimulation devices such as spinal cord stimulation (SCS) devices for pain, deep brain stimulation (DBS) devices for seizures, or intrathecal drug delivery systems – also is increasing significantly. There is growing likelihood that a patient with an implant will need an MRI sometime in his or her lifetime, but MRI scanning in patients with devices can potentially cause problems four ways: heating at the lead tip, rotational force (torque) on the device, functional impairment of electronics, and image distortion.
MRI-safe devices are in their very early stages, and Medtronic has the only FDA-cleared MRI-safe pacemaker system. In Europe, several companies have CE Marks for MRI compatible pacing devices. No MRI compatible ICDs have either a CE Mark or FDA clearance. In May 2013, Medtronic received a CE Mark for its CapSureFix Novus 5076 pacemaker lead when paired with an MRI-safe generator.
Other companies also are working to design new devices deemed safe in the MRI environment – referred to as MRconditional devices. However, there is some controversy about whether these new devices are really needed, and some scientists argue that MRIs can safely be performed on patients with existing pacemakers.
Interim findings from the MagnaSafe Registry in 2012 showed no important safety issues with existing devices, but there were some alterations in programming and some transient impedance changes during non-thoracic MRI in patients with pacemakers and ICDs. In 1, check 100 MRIs of patients with 816 pacemakers, 284 ICDs, and 214 leads (with 21% of patients pacemaker-dependent), there were no instances of imagingassociated death, device failure, generator or lead replacement, loss of capture, or electrical reset with MRI, which was performed consistently at 1.5 Tesla (T). That led some experts to conclude that most patients with conventional devices can undergo MRI scans.
GROWING NEED FOR MRI COMPATIBLE DEVICES
According to Medtronic, Germany and the U.S. have the highest rates of MRI procedures, at 97 per 1,000 patients and 91 per 1,000 patients respectively. In 2010, 29 million MRI scans were performed in Western Europe, with 6% of the population scanned each year, and that rate is doubling every 4-5 years. At the same time, >650,000 new pacing devices are implanted globally every year, making it fairly clear that an increasing number of patients with cardiac devices will need an MRI. A 2013 Sorin Group report said that MRI is indicated in 17% of all patients with pacemakers within 12 months of implantation.
Cancer survivors (12 million in the U.S.) are prime candidates for neuromodulation devices, according to Allen Burton, MD, of Houston Pain Associates and former chair of the pain medicine department at MD Anderson Cancer Center. He said that both cancer survivorship and chronic pain attributable to the disease itself or to its treatment are markedly increasing. The lack of MRconditional implantable neurostimulators has largely precluded their use for cancer pain, despite the fact that other treatments may not be as effective.
A common side effect of chemotherapy (especially platinum-based agents, such as the taxanes and vincristine) is peripheral nerve damage, resulting in burning, tingling, and pain in the feet that can be disabling. About a third of long-term cancer survivors have chronic pain, and Dr. Burton estimated that about a third of these have pain that is moderate-to-severe in intensity. Repeated surgeries, other nerve trauma, and poorly controlled radiation are other sources of chronic pain in cancer survivors. Dr. Burton said that the extent to which spinal cord stimulation (SCS) will alleviate that pain is unknown, but for other chronic foot pain patients, neurostimulators implanted in the mid-thoracic spinal cord level work up to 80% of the time. He added that MRI surveillance is used in cancer survivors to monitor for recurrence or spread.
MR:comp’s Schaefers said that among patients with spinal cord stimulators, 70 out of 100 are expected to require an MRI scan over the five-year life of a device, and the pattern is expected to be similar in the U.S. and Canada. A 2010 Medtronic study showed that for patients with implanted devices presenting in an emergency room, 39% got alternative diagnostic imaging, 35% had a spinal cord stimulation device explanted in order to get MRI imaging, and 0.7% of patients with an implanted SCS had an MRI despite contraindications.
The number of 3.0T MRI scanners is likely to increase, mainly for greater diagnostic potential in neurology. MR-conditional pacing systems have been tested at 1.5T, and implanted patients will probably be excluded from more powerful MRI scanners in the future. Furthermore, the MR-conditional pacemakers currently approved by the FDA are only dual-chamber devices. In the future, single-chamber pacemakers could be used even in permanent atrial fibrillation patients who don’t need a dual-chamber device. Thinner and better leads are also expected to result in more widespread and safe use of MRconditional systems.
Real-time MRI surgical procedures also are a coming trend, perhaps with patients no longer having to be awake during DBS because the quality will be so good that surgeons won’t need to talk to their patients. MRI Interventions, for example, recently received a $150,000 grant from the National Institutes of Health’s National Heart, Lung, and Blood Institute (NHLBI) to perform real-time, MRI-guided, catheter-based procedures in the heart.
MRI Risks
MRI exposure subjects patients to a static magnetic field, gradient magnetic fields, and an RF field. The static magnetic field produced by a 1.5T MRI scanner is 30,000 times stronger than the Earth’s magnetic field, according to safety expert Schaefers. The static magnetic field causes pulling and twisting of ferrous materials within the body and within the environment of the scanner which can cause device damage. In addition, patients may experience vibrations or other potentially disturbing sensations.
Gradient magnetic fields pulsed during imaging sequences can induce voltages on conductive structures with potential for unintentional stimulation of the patient and heating and damage to their device. The pulsed RF field, picked up by unintentionally created antennas in the body, may also create voltages and heating. The potential for RF heating near the electrodes is the primary concern in neurostimulation systems because the electrodes are in brain tissue, next to the spine, or next to peripheral nerves. Both device damage and unintended stimulation of a device are possible.
Current MR-conditional devices are safety rated mostly for 1.5T scanners. However, the use of newer 3.0T scanners is increasing, and they will require a new generation of tests and device adaptations. Steve Manker, program director for Medtronic Neuromodulation MRI-Conditionally Safe Systems, said, “We don’t know yet if the higher frequency will be worse or better. We need to do the testing. On the other hand, the shield technology is not tuned to a specific frequency, so we expect that it will perform quite well at 128 MHz.”
ACHIEVING “MR-CONDITIONAL”
There are three levels of MRI safety:
 MR-safe – This means the device is safe for use in MRI under all conditions. That is, the device is known to be safe or is made out of materials considered safe in the MR environment, such as plastic, silicone or glass, and poses no known hazards in all MR environments.
MR-safe – This means the device is safe for use in MRI under all conditions. That is, the device is known to be safe or is made out of materials considered safe in the MR environment, such as plastic, silicone or glass, and poses no known hazards in all MR environments. MR-conditional – This means the device poses no known hazards in a specified MRI environment with specific conditions of use, such as strength of the magnetic field, the spatial gradient, time varying magnetic fields, radiofrequency fields, and sometimes specific configurations of the device, including routing of neurostimulation system leads. Medtronic has incorporated three display icons into its SCS stimulator: MRI-CS full body scan eligible, MRI-CS head scan eligible, and MRI-CS eligibility cannot be determined.
MR-conditional – This means the device poses no known hazards in a specified MRI environment with specific conditions of use, such as strength of the magnetic field, the spatial gradient, time varying magnetic fields, radiofrequency fields, and sometimes specific configurations of the device, including routing of neurostimulation system leads. Medtronic has incorporated three display icons into its SCS stimulator: MRI-CS full body scan eligible, MRI-CS head scan eligible, and MRI-CS eligibility cannot be determined. MR-unsafe – MR unsafe is broken down into two subtypes – (1) unsafe because of the potential for movement or displacement or (2) unsafe because of the potential for induced currents, excessive heating, or other potential hazards. Manker said that Medtronic uses a shield-based technology for its SureScan SCS leads. While most device leads have a tubular body with four, eight, or 16 conductor wires inside the tube lumen, the SureScan tubular lead body is made up of two urethane layers sandwiching a braided metal layer. He added that implanted patients should be warned about possible harmless sensations of warmth, vibration, or even pulling and tugging during MRI scans.
MR-unsafe – MR unsafe is broken down into two subtypes – (1) unsafe because of the potential for movement or displacement or (2) unsafe because of the potential for induced currents, excessive heating, or other potential hazards. Manker said that Medtronic uses a shield-based technology for its SureScan SCS leads. While most device leads have a tubular body with four, eight, or 16 conductor wires inside the tube lumen, the SureScan tubular lead body is made up of two urethane layers sandwiching a braided metal layer. He added that implanted patients should be warned about possible harmless sensations of warmth, vibration, or even pulling and tugging during MRI scans.
Making a device MR-conditional includes getting heat to dissipate away from vulnerable tissues and components, using techniques such as Faraday cages to keep voltages away from vulnerable components and altering them in order to withstand voltages. Imricor Medical Systems, which makes MRI compatible electrophysiology tools, reportedly has a “special sauce” that it adds to leads in order “to avoid thermal and torsional aspects of risk.”
The Sorin Group report said that the key aspects of validating device compatibility with MRI are:
- Compatibility is linked within a system – device + leads.
- Worst-case conditions for testing to secure clinical
- Measurement certainty.
- Define equipment limitations.
- Diversity of potential adverse effects on the system.
- Organs temperature tolerance.
Manker noted that the first version of ISO/TS 10974:2012(E), a test specification standard that describes the appropriate tests for interactions between MR equipment and active implantable medical devices, was released in May 2012. The Association for the Advancement of Medical Instrumentation (AAMI), a non-profit organization founded in 1967, is working on international MRI safety standards.
If a company doesn’t have the internal expertise, it can turn to testing companies like Schaefers’ MRI:comp or Magnetic Resonance Safety Testing Services (MRSTS) to generate the MRI safety data necessary for regulatory approvals. Clinical trials are not always required, Manker said. The three levels of safety labeling icons and terminology for implant devices were established by the American Society for Testing and Materials (ASTM) International in August 2005. The ‘default’ assumed field strength that these categories apply to is 1.5T.
The three levels of safety labeling icons and terminology for implant devices were established by the American Society for Testing and Materials (ASTM) International in August 2005. The ‘default’ assumed field strength that these categories apply to is 1.5T.
Industry approaches
A 2013 Medscape article written by Luca Santini, MD, PhD, Giovanni Forleo, MD, PhD, and Massimo Santini, MD, said that in order to make its device MR-conditional, Medtronic redesigned the circuit protection normally applied to the power supply, the leads (to minimize and attenuate RF energy discharge at the tip), and the firmware, and the company changed the reed-switch to a Hall sensor.
There are a variety of strategies for circumventing potential lead vulnerabilities.
- Medtronic chose a shield-based technology for its SureScan SCS leads, Manker said. The design incorporates a Faraday cage, an enclosure that blocks external electrical fields in the outer wall of the lead tubing. The Faraday cage keeps the RF energy off the conductor wires and preferentially dissipates heat away from the spinal cord to the much larger surface area of subcutaneous tissue along the length of the lead and safely keeps temperatures low. As mentioned above, Medtronic’s SureScan tubular lead sandwiches a metal layer between two urethane layers.
- Boston Scientific’s Khalid Ishaque, international general manager for neuromodulation (pain and DBS), said that DBS leads must meet higher testing criteria, “In the brain, where there is risk of creating permanent tissue lesions, you can’t generate the heat that you can in the spine where spinal fluid will help to dissipate it.”
Ferrous materials pose a risk with an MRI scanner’s static magnetic field. Manker pointed out that not even Medtronic’s conventional leads contain ferrous materials. He explained that, due to conscious design choices, ferrous materials have been kept to a minimum in their stimulators and in control switches. He also said the stimulator electronics need to be robust to withstand voltages induced by the rapidly pulsing electromagnetic coils that produce the gradient field, and circuitry needs protection from the high radiofrequency energy that could harm the device components.
Current MR-conditional devices are safety rated mostly for 1.5T scanners. However, experts said the growing utilization of newer 3.0T scanners will require a new generation of tests and device adaptations. The 1.5T scanners produce RF energy at 64 MHz, and the 3.0T will produce RF energy at 128 MHz. Manker said, “We don’t know yet if the higher frequency will be worse or better. We need to do the testing. On the other hand, the shield technology is not tuned to a specific frequency, so we expect that it will perform quite well at 128 MHz.”
APPROVED DEVICES
MEDTRONIC
Medtronic has the only MR-conditional device approved for full body scans in the U.S., Canada, and Europe. No implanted neurostimulation devices are MR-safe – yet. MR scanners are rated according to Tesla strength, and current devices are too strong (1.5T) to be used on implanted patients. Manker said, “Since there are 7.0T and 9.0T systems coming, there is no way to guarantee safety in all MR systems.”
Medical devices with MR-safe labeling include some dental implants, shunts, and cosmetic implants, all of which are 100% non-metallic. Medtronic’s full body approval is for 1.5T scanners only. Because no devices can be labeled MR-safe in the neuromodulation market, the term MRI compatible is no longer used.
BOSTON SCIENTIFIC
Boston Scientific has the only neuromodulation device approved for the head in Europe, Canada, and Australia, but it is not cleared in the U.S. Ishaque said that some electrodes or leads will have design changes in order to get clearance for full body scans.
Boston Scientific and MRI Interventions (formerly SurgiVision) have collaborated since 2005 on both neuromodulation technology and implantable cardiac devices. Boston Scientific paid MRI Interventions $13 million in upfront licensing fees, with conditional milestone and royalty payments later.
Ishaque said, “We recognize that a system designed to allow full body MRI under certain conditions can be a valuable option for patients. We have MR-conditional labeling for the head in certain markets. We expect to continue to expand our MRI labeling over the next several years. Although we can’t disclose the exact timing, it is something we continue to work on.”
MRI INTERVENTIONS
The company’s ClearPoint system gives MRI-based stereotactic guidance for neurological procedures; it can be used in the hospital’s existing MRI suite and can be used with both 1.5T and 3.0T scanners. There are about 4,500 1.5T MRI scanners and 550 3.0T MRI scanners in U.S. hospitals. In 2010, the FDA cleared ClearPoint for general neurological procedures. In 2011, the company also got a CE Mark for the system.
MRI Interventions is working with several other companies besides Boston Scientific, including integrating the ClearPoint product line with Brainlab’s iMRI product line, focusing on drug delivery to the brain under MRI guidance.
CYBERONICS
The VNS Therapy System, a vagal nerve stimulator, is rated MR-conditional in the U.S. and in some other markets for imaging of the head and extremities, including knees. The U.S. clearance applies to both 3.0T and 1.5T scanners and is for the treatment of refractory epilepsy and treatment-resistant depression.
Milton Morris, PhD, Cyberonics senior vice president for research and development, said that his company’s device did not need to be modified for MRI safety, “For us, getting the labeling was an exercise in collaboration with the FDA and third parties (the University of Houston) over several years to demonstrate safety under specific conditions for both 1.5T and 3.0T scanners.”
Cyberonics plans to seek clearance for full body scans, but Dr. Morris said that there will have to be modifications in some leads and catheters for that. Cyberonics has a license agreement with Imricor Medical Systems to develop MR-conditional leads for the VNS System. Imricor’s main focus has been development of products enabling MR-guided cardiac ablation procedures, but the company is also working on other MR-conditional implanted devices.
Other
Four other companies in the space do not have approvals for MR-conditional devices but are interested in the area.
- St. Jude Medical. In June 2013 St. Jude made a $40 million equity investment in Spinal Modulation, receiving international distribution rights and an exclusive option to buy the company for up to $300 million. Spinal Modulation’s Axium Neurostimulator System is a neuromodulation device which targets the dorsal root ganglion in order to manage intractable pain in areas hard to treat with traditional SCS systems, including the lower leg, foot, and groin. St. Jude did not respond to repeated requests for information about this device.
- Spinal Modulation.
- Nevro.
- Greatbatch. In the areas of cardiac rhythm management and neuromodulation, Greatbatch has extensive intellectual property critical to enabling MR-conditional capability for implantable devices, according to Christopher Knospe, director of global communications. Greatbatch works with neuromodulation companies to make their products MRconditional. Greatbatch is working with St. Jude but would not discuss other customers/clients.
Through QIG, its subsidiary, Greatbatch is developing its own systems and devices. Greatbatch’s first complete medical device system, Algostim, is a spinal cord stimulation system to treat chronic pain of the trunk and limbs, developed in collaboration with two global leaders in neuromodulation, Richard North, MD, a neurosurgeon at Johns Hopkins University School of Medicine, and Giancarlo Barolat, MD, a Denver neurosurgeon.
Greatbatch is shopping for commercialization partners and plans to ask for FDA clearance and a CE Mark during the second half of 2013, according to Knospe. While the system is not MR-conditional, it was designed with the thought of applying for MR-conditional status down the line.
A Closer Look at Media Messages Versus Research Findings
Walter Alexander
The author is a freelance medical writer living in New York City.
It is generally reassuring when we read health advice that contains a clear message, especially when the advice involves something pleasurable. For instance, eat dark chocolate, and wash it down with red wine (in moderation). But confusion and consternation abound when research produces a mixed message that seems contrary to previous advice. After years of hearing that eating fatty fish or taking fish oil supplements was good for the heart, the eyes, and even mood, the public was puzzled this summer by a study that suggested a risk of prostate cancer in men with high levels of omega-3 fatty acids obtained from these sources.
Although “conclusions” in research are subject to change, in this instance, investigators not connected to the fish oil study complained that the headline-hungry media did not cover all of the facts. They also charged that the headlines were potentially harmful and that the findings were tainted by overreach. A closer look at the study is warranted.
WHAT THE RESEARCH SAID
In a paper published in July,1 Theodore Brasky, PhD, of the Ohio State University Comprehensive Cancer Center in Columbus and a team from the Fred Hutchinson Cancer Research Center in Seattle, Washington, found an association between higher plasma omega-3 fatty acid levels and an increased prostate cancer risk. Looking at data from the Selenium and Vitamin E Cancer Prevention Trial (SELECT) (clinicaltrials.gov Identifier NCT00006392), they measured plasma phospholipid omega-3 levels in 834 men who eventually developed prostate cancer and in 1,393 men who did not.
The men were classified according to their blood levels of three omega-3 fatty acids: eicosapentaenoic acid (EPA), docosapentaenoic acid (DPA), and docosahexaenoic acid (DHA). The researchers found that men in the highest quartile of overall omega-3 levels had, based on prostate cancer severity, an increased risk as follows: from 44% (low-grade cancer: hazard ratio [HR] = 1.44; 95% confidence interval [CI], 1.08–1.93) to 71% (high-grade cancer: HR = 1.71; 95% CI = 1.00–2.94).
Total prostate cancer risk was increased by 43% (HR = 1.43; 95% CI, 1.09–1.88). This finding echoed results from the same author’s 2011 research,2 leading the current Brasky team to conclude that long-chain omega-3 polyunsaturated fatty acids (PUFAs) were involved in prostate tumorigenesis. They said further that recommendations to increase long-chain omega-3 PUFA dietary intake should also address the potential risks.
Brasky et al. also pointed out that the strongest evidence that inflammation plays a role in prostate carcinogenesis is that the prostate cancer precursor lesion, proliferative inflammatory atrophy (an area of highly proliferative but atrophic epithelial cells), displays notable inflammatory infiltrates.(1) The group acknowledged, however, that studies of lifestyle factors associated with reduced inflammation (including the use of aspirin, nonsteroidal anti-inflammatory drugs, and statins) and the intake of long-chain omega-3 PUFAs (EPA, DPA, DHA) have been inconsistent. Obesity is associated with higher inflammation rates, a higher incidence of prostate cancer, and higher death rates. Counter to expectations, their own earlier 2011 study2 had found that:
- high levels of serum phospholipid long-chain omega-3 fatty acids (a biomarker of usual omega-3 fatty acid intake), were associated with a large increase in the risk of high-grade prostate cancer.
- high levels of trans-fatty acids (associated with increased inflammation) were associated with a reduced risk of high-grade prostate cancer.
These findings, the authors write, were a stimulus for the current study,(1) because they raise the possibility that high intakes of omega-3 fatty acids through fish oil supplements, for example, could significantly raise the risk of high-grade prostate cancer. In light of the widespread use of omega-3 fatty acid supplements, the purported health benefits of eating fatty fish, and ongoing clinical trial testing of omega-3 fatty acid supplementation for the prevention of cancer and cardiovascular disease, an investigation of a possible contribution to prostate cancer risk becomes especially important, they said.
WHAT THE MEDIA REPORTED
In an NBC News Health article,3 Dr. Brasky is quoted as stepping somewhat beyond the bounds of the conclusion in the 2013 journal article,1 suggesting that for some men, taking “mega, mega” doses of fish oil supplements is “probably a little bit dangerous.”
The NBC article also notes that whereas the American Heart Association recommends eating fish twice weekly and perhaps taking fish oil capsules for those with heart disease, recent studies have shown that taking extra omega-3 fatty acids has little effect on heart disease.(3) The article also mentions that the researchers did not consider fatty acids in vegetable oils to be related to prostate cancer risk.3
In a study reported in the May 2013 issue of the New England Journal of Medicine,(4) among 12,000 patients with heart disease but without a history of a heart attack, 1 g daily of omega-3 fatty acid supplementation did not reduce morbidity or mortality rates. Therefore, for men hesitant to change course, given that heart disease is much more common than prostate cancer, the shadow of doubt cast on the omega-3’s cardioprotective effects might be a decisive factor.
For William Harris, PhD, Professor of Medicine at University of South Dakota School of Medicine in Vermillion, and a senior scientist at Health Diagnostic Laboratory, Inc., in Richmond, Virginia, decisions triggered by such reports are a real concern. He said in an interview:
Many people with hypertriglyceridemia who are put on prescription fish oils might be tempted into not taking them—and that’s wrong. Also, vastly more individuals are taking fish oil supplements and like to eat high omega-3 fish because they think it’s good for them. The message they are getting now—that omega-3 is in general bad—is incorrect.
In a MedCity News article,5 Dr. Harris emphatically agreed with that statement, charging that although the Brasky study1 certainly had validly added to the prostate cancer evidence base
on omega-3 fatty acids, that team and the media coverage had “extrapolated the findings far beyond the data themselves.”
The unsupportable extrapolation, he said, is “that omega-3 intake causes an increase in prostate cancer risk. … Correlation does not imply causation.”
Dr. Harris pointed out that Brasky et al.(1) provided no data on fish intake or supplement use. So the question of whether fish oil supplements or an intake of more oily fish increases
prostate cancer risk was not tested.
In a further critique of the Brasky article, published on LecturePad,(6) he listed eight major randomized clinical trials (Table 1) of omega-3 fatty acid supplementation that reported incident cancer diagnoses or cancer deaths, with a total enrollment exceeding 78,000 subjects. The list showed small increases in cancer diagnoses or cancer deaths in six of the eight trials, but the increases for omega-3 fatty acid supplementation did not reach statistical significance in any of the trials.
Dr. Harris cited extensive literature on fish intake and higheromega-3 fatty acid intake that demonstrated a lower incidence of prostate cancer incidence and death, better survival among men who already had prostate cancer, and a reduced riskof aggressive prostate cancer. Furthermore, citing World Foundation of Urology data,7 he noted that the incidence of prostate cancer is high in North America and Northern Europe (among Caucasians and African-Americans (63 and 102 per 100,000, respectively) but low in Asia. With the Japanese intake of omega-3 fatty acids at about eight-fold that of Americans and with their blood levels twice as high, one would expect a higher risk. However, the Japanese prostate cancer rate of 22.7 per 100,000 in 2008 was dramatically lower than the U.S. rates of 83.8 per 100,000.(8)
The Brasky article stated that the mean percentage of total omega-3 fatty acids (EPA + DPA + DHA) was 4.66% (range, 4.56%–4.75%) in cancer patients.(1)
“These omega-3 levels,” according to Dr. Harris, “were far lower than would be expected from individuals taking omega-3 supplements.”
The Brasky paper showed significantly lower omega-3 (EPA DPA + DHA) levels in men without prostate cancer at 4.48% (range, 4.41–4.55; P = 0.002).1 The clinical significance of that difference (from 4.48% to 4.66%) was questioned by Richard Deckelbaum, MD, Director of the Institute of Human Nutrition at Columbia University in New York City. He explained in an interview:
I specialize in fatty acid levels, and I was surprised at how small the omega-3 fatty acid differences are, especially for EPA, DPA, and DHA. In our lab, we would not consider these small differences to be biologically significant. Because of the large number of subjects in the SELECT trial, it turned out to be statistically significant, though.
He speculated that perhaps prostate cancer itself could cause these “very small” changes in fatty acid levels. He said, “It’s not quite clear as to where the chicken is and where the egg is.”
Of note, Dr. Harris mentioned the same possibility—that higher levels of omega-3 fatty acids in prostate cancer could be “an innocent bystander.”
Dr. Deckelbaum noted that omega-3 fatty acid intake in North Americans is generally lower than it should be, and he urged that people follow the American Heart Association’s
recommendation to increase omega-3 intake.
Regarding the conclusions drawn from the analyses in Brasky, he said, “I certainly would have been more cautious and would not have made recommendations based on them.”
OMEGA-3 INTAKE VERSUS OMEGA-3 LEVELS
A majority of recent observational studies, said Eliot A. Brinton in an interview, have shown that at least DHA levels— and possibly EPA levels—are associated with certain types of prostate cancer. Dr. Brinton is Director of Atherometabolic Research at Utah Foundation for Biomedical Research and Associate Professor at the University of Utah School of Medicine in Salt Lake City. There does appear to be a difference between EPA and DHA levels in that association, he said.
Brasky et al. reported mean DHA levels (a percentage of the total) of 2.91% in subjects with no cancer and 3.09% in those with high-grade prostate cancer (P = 0.009). For EPA, the mean
levels were 0.61% and 0.65%, respectively (P = 0.40). For DPA they were 0.86% and 0.89%, respectively (P = 0.16). However, Dr. Brinton added that studies of dietary intake of fish oil tend to show an opposite protective relationship with respect to prostate cancer.
“So we are left with an apparent contrast between certain levels of omega-3 and intake of omega-3,” he said.
Dr. Brinton emphasized that no randomized, controlled clinical trial data point one way or the other. The available dietary intake studies, he said, are observational:
You are just asking people what they ate, so these observational studies are just hypothesis-raising—and there we find heterogeneity between EPA and DHA, while the controlled clinical trial data are inconsistent. The best we can tell is that intake is good— and that’s hypothesis-raising—and we only say there’s a lot of confusion regarding what the levels are trying to tell us.
The results of REDUCE-IT (Reduction of Cardiovascular Events with EPA–Intervention Trial) may help to elucidate the issues, Dr. Brinton said. In that ongoing randomized trial, icosapent ethyl (Vascepa, Amarin) capsules, at 4 g/day, or placebo is added to statin therapy in high-risk patients with hypertriglyceridemia (fasting triglyceride levels of 200 to 500 ml/dL) and coronary artery disease (CAD) or CAD risk factors. Vascepa contains only EPA. (Icosapent ethyl is a high-purity prescription form of EPA ethyl ester.) The primary endpoint includes cardiovascular events. REDUCE-IT is being conducted at almost 300 international sites with a target enrollment of about 8,000 patients, with completion anticipated in 6 years. Dr. Brinton is on the trial’s steering committee and has been a speaker and consultant for Amarin.
Although several earlier trials and studies have supported cardioprotection with omega-3 intake, some recent trials of low-dose EPA plus DHA have failed to show that association.
“The ongoing REDUCE-IT trial may resolve whether or not higher doses of pure EPA reliably reduce CVD,” Dr. Brinton said.
His main concern, however, was that the public reporting on the research of the Brasky findings—which clearly did not address fish intake—linked fish intake with prostate cancer.
“They got it all wrong,” he said. The result of these contradictory messages about omega-3 fatty acids, cancer risk, and heart disease? “The public is whipsawed,” he said. Dr. Brinton voiced uneasiness, as well, that the researchers did not adequately highlight some “striking heterogeneity” in their meta-analysis of prospective biomarker studies measuring associations between EPA; DHA; long-chain omega-3 PUFAs; and total, low-grade, and high grade prostate cancer. In each category of cancer type for each of the three omega-3 fatty acids, one or two studies out of four to seven showed positive effects on events—for instance, a relative risk of 0.53 for high-grade cancer with DHA, as stated in the study by Charvarro et al.(9) “I wish they had addressed that,” Dr. Brinton said. He speculated that the puzzling turnaround in cardiovascular outcomes with omega-3 studies might be related to the effective contemporary use of beta blockers, antiplatelet therapy, and statins, making it much more difficult to show benefit from omega-3 fatty acids. Even though these same studies failed to show cardiovascular benefits of fish oil, along with studies showing a possible association between prostate cancer with higher omega-3 levels, Dr. Harris strongly believes that the benefits of a higher intake of omega-3 fatty acids outweigh any possible harm. With the National Vital Statistics report for male prostate cancer deaths at 28,500 in 2010 and 207,500 for ischemic heart disease in the U.S., what he called a “conservative” estimate of a 10% reduction in heart disease death risk stacks up well against a “liberal” assumption of a 50% increase in prostate cancer deaths. Under that model, the chances of dying from ischemic heart disease are still nearly 4.5 times greater that the risk of dying from prostate cancer. “The wealth of data in other prostate cancer studies point in the direction of showing protective effects of omega-3 fatty acids,” he added. Dr. Harris concluded that the study authors and the media alike should discipline themselves to report findings in a balanced context and should “resist the temptation to wildly extrapolate in order to grab headlines”—especially if failing to do so puts patients at risk, he said.
NUMBERS HAVE CONSEQUENCES
The numbers pertaining to prostate cancer remain compelling. The American Cancer Society projects that almost 239,000 new cases of prostate cancer will be diagnosed in 2013 and that nearly 30,000 men will die of this disease. During his lifetime, a man stands a 1 in 6 chance of having prostate cancer.
Dr. Brasky told NBC Health, with regard to his message about fish intake, given the 70% increased risk in high-grade prostate cancer, “I think it’d be a concern for people.”3
Dr. Brinton said, “My bottom line is, ‘keep eating fish.’ ”For Dr. Harris, the critical fact is that omega-3 fatty acids are associated with a reduced risk of the leading cause of death in men and women in the U.S.—cardiovascular disease.
Currently approved omega-3 agents include icosapent ethyl (Vascepa) with EPA only, and omega-3-acid ethyl esters (Lovaza capsules, GlaxoSmithKline), with 47% EPA and 38% DHA. Epanova, Omthera’s investigational drug, contains EPA (range, 50%–60%) and DHA (range, 15%–25%). Phase 3 studies have been completed. AstraZeneca purchased Omthera in May 2013.
REFERENCES
- Brasky TM, Darke AK, Song X, et al. Plasma phospholipid fatty acids and prostate cancer risk in the SELECT trial. J Natl Cancer Inst, July 10, 2013 (online).
- Brasky TM, Till C, White E, et al. Serum phospholipid fatty acids and prostate cancer risk: Results from the prostate cancer prevention trial. Am J Epidemiol 2011;173(12):1429 1439.
- Fox M. Fish oils may raise prostate cancer risks, study confirms. NBC News Health, July 10, 2013. Available at: www.nbcnews. com/health/fish-oils-may-raise-prostate-cancer risks-studyconfirms- 6C10597283. Accessed August 5, 2013.
- The Risk and Prevention Study Collaborative Group. n-3 fatty acids in patients with multiple cardiovascular risk factors. N Engl J Med 2013;368:1800–1808.
- MedCity News. The omega-3/prostate cancer media fiesta:
Mistaking correlation for causation puts patients at risk. July 16, 2013. Available at: http://medcitynews.com/2013/07/theomega- 3prostate-cancer-media-fiesta-mistaking correlationfor- causation-puts-patients-at-risk. Accessed August 5, 2013. - Harris W. Problems with recent study on omega-3 fatty acids and risk for prostate cancer. Available at: www.lecturepad.org/ index.php/commentaries-and-opinions/1153-omega-3-fattyacids- and-risk-for-prostate-cancer. Accessed August 5, 2013.
- World Foundation of Urology. Prostate cancer prevention. Available at: www.prostatecancerprevention.net. Accessed August 15, 2013.
- World Health Organization, International Agency for Research on Cancer. Globocan 2008, Cancer Fact Sheet. Prostate Cancer Incidence, Mortality and Prevalence Worldwide in 2008 Summary. Available at: http://globocan.iarc.fr. Accessed August 7, 2013.
- Chavarro JE, Stampfer MJ, Li H, et al. A prospective study of polyunsaturated fatty acid levels in blood and prostate cancer risk. Cancer Epidemiol Biomarkers Prev 2007;16(7):1364–1370. n
A staggering 99% of prostate cancer patients treated with proton therapy believe they made the best treatment decisions for themselves, according to a new report released today at the National Proton Conference in Washington, D.C. The report analyzed outcomes and satisfaction of approximately 6,400 prostate cancer patients, more than 80% of whom received treatment at Loma Linda University Medical Center’s (LLUMC) James M. Slater Proton Treatment and Research Center.
“This report reaffirms the results we’ve seen from our patients for the past 22 years and supports the mountain of evidence regarding the efficacy of proton therapy,” said Jerry D. Slater, M.D., chairman of the LLUMC center. Dr. Slater and Dr. David A. Bush, vice-chairman of the department of radiation at LLUMC, recently co-authored a similar study entitled “Multi-Institutional Patient-Reported Quality of Life After Proton Therapy for Prostate Cancer Compared to Non-Treated Men.”
The just-released report was commissioned by the National Association for Proton Therapy (NAPT) and conducted by Dobson DaVanzo & Associates, LLC, an independent health economics and policy consulting firm. It looked at patient-based outcomes analysis and included personal questions that provided meaningful data that helps physicians make treatment decisions.
Not only did approximately 99% of the patients surveyed believe they made the best treatment decision for themselves, but an almost equal number – almost 98% – reported that they had recommended proton therapy to others.
Additional key findings of the report included:
- Approximately 96% of patients were • satisfied or extremely satisfied with proton therapy.
- Ninety-two percent of patients • reported that their quality of life was better or the same today than it was before their treatment. Only 8% stated that their quality of life was worse.
- Ninety-two percent of respondents • reported that physical health or emotional problems did not interfere, or interfered very little, with their social activities.
- Those who completed proton therapy • for the treatment of prostate cancer had similar urinary, bowel and hormonal health-related quality-of-life (HRQOL) measures compared to healthy individuals. For patients who received hormone therapy in addition to proton therapy, lower sexual HRQOL measures were reported. However, when looking at patients who received only proton therapy for the treatment of prostate cancer and who did not receive hormone or photon therapy, proton therapy patients reported lower HRQOL than healthy individuals in only one category, “sexual bother,” which refers to annoyance related to their sexual symptoms.
In addition to prostate cancer, proton therapy is effectively used to treat many different types of cancer. The outcomes of the NAPT report can be attributed to the pinpoint accuracy of the highly targeted proton beams. According to Dr. Slater, “Proton therapy is extremely effective as a treatment for prostate cancer because the targeted proton beams spare surrounding healthy tissue and minimize the typical side effects from standard photon beam radiation including incontinence and impotence.”
Since LLUMC introduced modern proton treatment for cancer into the mainstream in 1990, there have been countless studies and trials that have shown proton therapy to be the treatment of choice for many types of cancer. Over the years proton treatment has been refined and, coupled with leading-edge technology, has become one of the best treatment options for doctors and patients. While prostate cancer remains one of the primary uses for proton therapy, the pinpoint accuracy of the proton beam also makes it a highly effective form of treatment for many other types of tumors including those found in the head, neck, lung and breast.
Source: News Release.
Back to Phase 1: Understanding Systemic Effects of PV-10
The expression “bench to bedside” describes the progression from basic laboratory and animal research into disease and therapeutic processes through to “translational” studies that test human clinical applications suggested by those initial investigations. Sometimes, though, the arrow points the other way — “from bedside to bench,” for example, when promising clinical findings of apparent health benefits demand more granular and comprehensive understanding. That is the case in a Phase 1 study of a treatment for metastatic melanoma being conducted under Amod Sarnaik, MD, of the Experimental Therapeutics Program at the H. Lee Moffitt Cancer Center and a faculty member at the University of South Florida.
The therapy under investigation is intralesional PV-10 (Provectus Pharmaceuticals). PV-10 was developed from Rose Bengal, a xanthene dye combining halogens with fluorescein, patented in the 1880s. Before its antineoplastic potential was discovered and developed, it was used medicinally to fight eye infections, for staining, as an intravenous assay for impaired liver function, and as a food dye.
Back in October, 2012, Phase 2 metastatic melanoma data1 on use of intralesional PV-10 presented at ESMO (European Society for Medical Oncology) 2012 Congress in Vienna, Austria, showed an objective response rate (ORR) of 51%, and a disease control rate of 69% in target melanoma lesions. The other finding, which lies behind some of the intensifying interest in PV-10, was a 61% ORR in bystander (uninjected) lesions among patients who had complete or partial responses in their target lesions. The bystander lesion ORR in patients with nonresponsive target lesions was 18%. Of deep interest, as well, were case studies showing potential stasis or regression of untreated visceral lesions in patients following PV-10 treatment of their cutaneous lesions.
While PV-10 is known to be excluded from normal cells, it accumulates in the lysosomal membranes of cancer cells. There it subsequently triggers lysosomal release and complete autolysis of tumor cells relatively quickly–within 30-60 minutes of the injection. Importantly, this acute necrosis of the treated tumor does not appear to denature tumor antigens, potentially allowing acute exposure of antigenic tumor fragments to antigen-presenting cells.
Murine evidence
In murine research, Paul Toomey, MD, also of Moffitt, and colleagues used B16-F10 melanoma cells to establish a solitary subcutaneous flank tumor and multiple lung metastases in one study, and in a second study, bilateral flank tumors. When investigators administered a subcutaneous PV-10 injection to the flank tumor in the first study and a PV-10 injection in one of the tumors in the second, tumor size was reduced significantly. A bystander effect was clearly apparent in the first study in that PV-10-treated-mice had 3 or fewer lung metastases as compared with more than 250 in each of the untreated mice. Also, tumor-specific interferon (IFN)-? production was significantly higher (p 5 0.05) in the PV-10-treated mice. IFN-? is a cytokine that is critical for innate and adaptive immunity for tumor control. The overall conclusion, Dr. Toomey said, was that “intralesional PV-10 treatment leads to direct chemoablation of melanoma lesions and to a systemic response.”
Seeking an immune cell infiltrate
To find direct evidence of such a systemic immune response is part of the motive behind heading back to the bench—although this time involving human subjects. “A further impetus toward teasing out the precise mechanism of how PV-10 can exert a systemic immune response in patients,” said Dr. Sarnaik in an interview, “is to allow us to rationally combine PV-10 treatment with some of the exciting emerging immunotherapies for metastatic melanoma.”
The focus at Moffitt, Dr. Sarnaik continued, is on discerning the presence of immune cell infiltrate in untreated tumors after PV-10 injections into other lesions. “We are really interested in harnessing immune cell infiltrate as a form of treatment,” he said, noting also that while creating cancer vaccines has been thought of traditionally as one of the Holy Grails of cancer research, cancer vaccines have turned out to be not strong enough to generate an adequate immune response.
Adoptive cell transfer
The strategy of adoptive cell transfer potentially overcomes the weak vaccine response. With adoptive cell transfer, antigen-specific effector cells are taken from the patient’s tumor and expanded ex vivo under laboratory conditions favoring growth of T-lymphocytes and then re-infused to the patient. This precludes the need to provide antigens or to activate antigen-presenting cells.
In melanoma, T-cells from the tumor are cultured from tumor resection specimens in the presence of interleukin-2.A second strategy infuses peripheral blood T-cells that have been genetically engineered to express tumor-antigen-specific T-cell receptors2.
While adoptive cell transfer offers the advantage that enough T cells can be obtained for infusion in all patients, the T-cell receptors transfected into the T cells have a limited antigen-specificity. The strategy works, Dr. Sarnaik said, only about half the time. “We generate large numbers of T-lymphocytes, but we don’t have control over their quality. We think one of the limitations is that the T cells you get out of the tumor just aren’t good enough.” PV-10, however, does cause an immune response, suggesting that a combination treatment may improve the quality of the T-lymphocytes and have a greater impact on the disease.
When Shari Pilon-Thomas, PhD, also a Moffitt researcher, demonstrated that T-lymphocytes recovered from mice treated with PV-10 do appear to be of a higher quality, as evidenced by stronger tumor reactivity, the stage was set for Dr. Sarnaik’s current 15-patient pilot study. In it, one of two resectable melanoma tumors is injected with PV-10. Both are removed several weeks later. Serum is assessed before and after treatment to look for changes in the infiltration of immune cells. In patients with an immune response, PV-10 therapy can be continued.
“This is a straightforward study that will give a yes or no answer,” Dr. Sarnaik said.
Investigators will monitor carefully for known PV-10 adverse events, such as strong sun sensitivity, and interactions with diuretics, older psychiatric medications and some topical agents. Because drug concentrations are high only locally, intralesional therapy produces limited toxicities. The study will be completed in a year, with data analysis requiring another 6 months. First results may be ready in a year, however.
If the hypothesis that PV-10 will produce a better immune cell infiltrate is borne out, that would justify testing of combination treatments, Dr. Sarniak said. Likely candidates are adoptive cell therapy, approved drugs like ipilimumab that boost immune response, or PD-1-blocking antibodies (none approved yet).
What kind of therapy is PV-10?
Echoing Dr. Sarnaik, Eric Wachter, PhD, Provectus chief technology officer, said that he hopes that the findings of Dr. Sarnaik’s study will point toward rational judgments about combining PV-10 with other documented therapies. “We then might want to try two or more orthogonal therapies to stress tumor cells from several different angles simultaneously, for example an immune therapy plus a metabolic therapy (e.g., a kinase inhibitor), or in a rationally designed sequence.” In a hepatocellular carcinoma model, he added, PV-10 showed significant potential for synergy with 5-fluorouracil. Provectus recently initiated clinical testing of PV-10 with the multikinase inhibitor sorafenib, again bringing in two therapies with divergent mechanisms of action.
Which category does PV-10 fall into? “I think we are getting a clearer picture of how it might be classified, but it has features of several previously unrelated categories, such as of adoptive cell transfer and vaccination,” Dr. Wachter said. “PV-10 initially reduces tumor burden through chemoablation—but then activates the immune system bringing in capacities completely orthogonal to the ablative tumor destruction,” he added.
“Amod Sarnaik’s work may give us the molecular basis for closing the loop on one of the founding concepts for going into the clinic in the first place,” Dr. Wachter commented. “Back in the preclinical days at Provectus, Craig Dees, PhD, theorized that ablation of tumors with PV-10 might lead to unmasking of tumor antigenic material. I don’t think he anticipated that it would work as well as it does.”
Further testing
A Phase 3 randomized trial comparing PV-10 with dacarbazine and temozolomide monotherapy is expected to begin enrolling patients in Australia, the US and Europe later this year. The trial will include approximately 200 subjects with stage IIIB and IIIC melanoma and will have progression-free survival as its primary endpoint.
1) Sanjiv Agarwala, M.D., abstract #1137P, “Immuno-chemoablation of metastatic melanoma with intralesional rose bengal.”
2) W. Joost Lesterhuis and Cornelis J. A. Punt. “Harnessing the immune system to combat cancer.” 2012. Nature Reviews/Drug Discovery. Supplement to Nature Publishing Group Journals.
Synthetic Circuit Allows Dialing Gene
Expression Up or Down in Human Cells
Scientists who built a synthetic gene circuit that allowed for the precise tuning of a gene’s expression in yeast have now refined this new research tool to work in human cells, according to research published in the February 5, 2013 online issue of Nature Communications.
“Using this circuit, you can turn a gene from completely off to completely on and anywhere between those two extremes in each cell at once. It’s a nice tool if you want to know what happens at intermediate levels of gene expression. There has been no such system so far, but now it is available for mammalian cell research,” said senior author Gábor Balázsi, Ph.D., associate professor in The University of Texas MD Anderson Cancer Center Department of Systems Biology.
Present options for altering gene expression in human cells are blunt instruments by comparison. Knocking out a gene eliminates its expression completely. Inhibiting it with RNA interference dials it partially down and can affect other genes. Inserting a gene expression vector into cells overexpresses the gene, but it’s usually uncontrolled. Commercially available versions can switch a gene on or off, but cannot precisely dial between these extremes.
“For cancer research, the system will allow scientists to test the boundaries of a gene known to confer resistance to a drug in cancer cells by dialing its expression to different levels and treating the cells with the drug,” said first author Dmitry Nevozhay, M.D. Ph.D., instructor in Systems Biology.
“Likewise, such a system would allow personalized gene therapy, by precisely tuning the therapeutic gene level expression depending on disease progression and the patient’s need,” Nevozhay said.
In microbial or yeast biology research scientists have started to understand and manipulate gene function quantitatively, almost like we understand electronic circuits, Balázsi said. “This makes research in those areas more amenable to engineering and mathematical characterization, but that’s not true for human cells, and part of the problem is that tools that tune gene expression have been lacking.”
A step-by-step guide for others to build mammalian synthetic gene circuits
By refining their circuit to work in a human breast cancer cell line, the team demonstrated that their approach can be used in mammalian cells while offering a step-by-step guide that other researchers could follow to build other synthetic circuits for use with other genes.
CANCER WATCH, VOL. 22, FEBRUARY 2013
By: Walter Alexander
One of the real impediments to wider acceptance of alternative and anthroposophical medications and approaches to treatment has been the nearly utter lack of high standard randomized clinical trials showing benefit. In the world of conventional medicine, the randomized controlled trial (or RCT) is the Holy Grail of validity. Without RCTs, claims for benefits based on individual experience have not been taken seriously.
In such trials, one group gets a specific treatment and a similar randomly chosen other group gets a sugar pill or placebo. To attain the highest level of scientific acceptance, an RCT needs also to be both prospective and double-blind, as well. That means that the question to be tested has to be explicitly stated before the start of the trial (no fishing for favorable effects afterwards allowed!), and neither the physicians nor the patients know who got the real treatment until after the trial has been completed and “unblinded.”
With that, there are serious impediments to launching and carrying out RCTs. They are enormously expensive to conduct, such that often only the huge pharmaceutical companies with colossal research budgets can afford them. Furthermore, only those drugs or procedures likely to produce the immense profits needed to offset those costs get tested.
In addition, as the author of the first study below points out, patients may not want to be randomized. Asked whether or not they would submit to randomization and subject themselves to the 50-50 odds of getting a placebo, 97 percent of the patients in the anthroposophical treatment group said no. The first serious rebellion against RCTs occurred early in the HIV/AIDS crisis when legions of HIV positive individuals agreed to enter them in order to get the latest treatments, only to run to friendly chemists to have their pills tested. If they were sugar, they dropped out of the trial and explored new treatments elsewhere.
All this amounts to a “Catch-22” of the first order. David Riley, MD, University of New Mexico School of Medicine and Integrative Medicine Institute, Sante Fe, New Mexico, has long been an advocate of alternative clinical trial designs that would allow smaller clinical practices to participate in valid research at lesser expense, and help overcome the very serious lack of supportive data for alternative and complementary therapies. He was a secondary author in the first trial reported below. This trial, rather than testing a drug against a placebo, prospectively tests two approaches to treatment for the same extremely common ailments: acute respiratory tract infections (RTI) and acute ear infections (otitis media, or AOM).
The author, Harald H. J. Hamre, MD, of the Institute for Applied Epistemology and Medical Methodology, Freiburg, Germany, points out in his introduction that RTI and AOM are very common in primary care practice and that most patients are prescribed an antibiotic. The use of antibiotics for RTI/AOM, however, is not supported by clinical trial experience. In fact, large data reviews show that compared to their potential to produce undesirable side effects, the benefits of antibiotics in AOM, sinusitis, tonsillitis, common cold and bronchitis are small or negligible. Beyond side effects, their indiscriminate use promotes bacterial resistance. Hamre explains also that in anthroposophic medicine, RTI/AOMs are treated with an array of medications supported by external herbal and hydrotherapeutic applications. Antibiotics are avoided unless “strongly needed,” and fever is not routinely suppressed with analgesics.
The non-randomized study, entitled “Anthroposophic versus Conventional Therapy of Acute Respiratory and Ear Infections” (Wien Klin Wochenschr, 2005, 117/7-8: 256-268), evaluated treatment in “real-world” clinical practices in Austria, Germany, Netherlands, UK and the United States. Practices were either anthroposophic or conventional. Specific treatments were left to the physicians’ discretion. The study objective was to compare clinical outcomes, medication use and patient satisfaction, testing the hypothesis that clinical outcomes would not be worse with anthroposophic treatment than with conventional. The primary endpoint was response, defined as a complete recovery or major improvement, after 14 days.
The analysis included 1016 patients treated by 36 physicians (715 treated by anthroposophic doctors and 301 by conventional). The response rate for anthroposophic treatment was not only non-inferior to conventional therapy (89.7 percent versus 84.4 percent for conventional), it was significantly superior. Responses and complete recovery were more frequent and faster. Subanalysis, however, showed that the differences were accounted for by stronger results in children receiving anthroposophic treatment, with comparable findings for both therapies in adults. Also, significantly more anthroposophical patients were satisfied with their treatment. Adverse drug reactions were reported in 2.7 percent of anthroposophic patients and in 6.0 percent of conventionally treated patients.
The study showed, Hamre concluded, that anthroposophic treatment of primary care patients with acute respiratory and ear infections is safe and at least as effective as conventional treatment. “In addition,” he wrote, “anthroposophic treatment allows for a very low use of antibiotics, analgesics and anti-inflammatory drugs.” In fact, about 36 percent of conventionally treated patients took antibiotics as compared with about 6 percent of anthroposophically treated patients.
Some caution is called for in interpreting the data. Anthroposophically treated patients may well have been more motivated. Hamre noted that such treatment often calls for more frequent dosing and intensive nursing, and it has to be allowed that the self-selection by patients treated via the anthroposophic approach may invite a bias in their own reporting.
The second clinical trial report, Anthroposophic therapies in chronic disease: the Anthroposophic Medicine (AM) Outcomes Study (AMOS) (Eur J Med Res, 2004 9:351-360), also conducted as a “real world” observational study under Hamre, included the wider, multi-modal range of anthroposophical remedies, encompassing both anthroposophical medicines and art, movement (eurythmy) and massage therapies. There were no comparator groups. The primary comparisons were internal, assessing aspects of status at entry and at specific time periods thereafter (i.e., disease severity and health-related quality of life). Secondary outcomes included costs and therapy and health utilization, where the prior years were compared with the first AM treatment year.
The most common diagnoses were mood disorders, fatigue, low back pain, headache, cervical spine disease, asthma, malignancies and attention deficit/hyperkinetic/conduct disorders. Analysis at 24 months of data from 811 patients (age 1-75) showed “substantial, consistent and stable improvements of disease symptoms and health-related quality of life.” Therapy costs were outweighed by savings attributed to reduced hospital stays. Adverse reactions to therapies were few (2.7 percent) and rarely caused dropout (0.5 percent).
Hamre concluded, “Anthroposophic therapies were associated with substantial long-term reduction of disease severity and improvement of health-related quality of life.” He said also, “Considering the long disease duration before enrollment (average 6.5 years), these results are encouraging.” In his discussion of the implications of the study, Hamre pointed out that patients often gave as their reason for consulting an AM physician, aside from perceived shortcomings of conventional therapies, a desire to contribute actively to therapy. “Anthroposophic counseling and therapy for chronic disease aims to affect underlying causes of the patient’s condition, which may not be addressed adequately through passive therapies,” Hamre observed.
Dr. Hamre’s final comment here is important. Conventional research design strives mightily to overcome the problem of “the placebo effect,” that often huge component of outcomes seemingly caused by the patient’s awareness that she or he is receiving treatment. Conventional medical researchers are often chagrined that placebo effects greater than 20 percent are frequently documented as confounding factors in their analyses. The further element of active engagement by the patient is another dimension that refuses to remain ignored. Highly regarded conventional research into the impact of support groups for women treated for breast cancer has shown remarkable benefits. Acceptance of the notion that when patients activate their own will forces in relation to their medical condition, they can set in motion powerful physiologic changes, has not truly arrived. But resistance to it is weakening, and serious consideration of it is implied in these studies of anthroposophic approaches to treatment.
Wednesday, 12 December 2012 16:58
By Walter Alexander, Contributing Writer – Vol. 13, No. 4. Winter, 2012
Escape Fire: The Fight to Rescue American Healthcare is not the first documentary to bemoan the inadequacies of healthcare here in the US. But it is unique and commendable for the way it looks at potential solutions already known in “real world” practice.
Before exploring ways out, Escape Fire does provide the de rigueur cold water bath of unpleasant healthcare cost data, personal health tragedies, practitioner entrapment, and political/social deadlock. The arc of current cost expansion, if followed unabated, is projected to gobble up $4.2 trillion annually (~20% of our gross domestic product) in ten years. At present, US yearly expenditure on pharmaceutical drugs (about $300 billion) nearly matches the amount spent by the rest of the world.
The rationale for the film’s title is explained by Don Berwick, MD, former Medicare/Medicaid head. It derives from a life-saving strategy invented on-the-spot by a forest fire fighter trapped with fellow smoke-jumpers in the midst of a wildfire speeding uphill towards them. He throws a match to create a safe burned out area, and begs his fleeing companions to join him. They do not listen, and most of them perish, while he survives nearly unscathed.
The analogy the filmmakers propose is that while our healthcare system is “burning up around us,” rescue solutions are already before us, but people are so embedded in the status quo that tragically they can’t recognize viable escape strategies even if they’re staring them in the face.
Intellectually, the analogy is a bit weak but the directors have documented some impressive and frightening “flames.”
Case in point is Erin Martin, MD, a general practitioner on her last day at a low-income primary care clinic in Oregon. She resigns because of the demoralizing effect of her 25-patient per day schedule. At the same time that she despairs she cannot devote the time needed to truly help her patients, the clinic administration is constantly asking her, “How can you get your productivity up? You need to see more patients because we’re in the red.”
Directors Matthew Heineman (Emmy nominated) and Susan Froemke (four-time Emmy winner) follow Dr. Martin as she finds her way to the University of Arizona’s Program in Integrative Medicine, and then to a Washington State community clinic that is physician owned and operated and that promised her the ability to shape her own practice.
There she now can devote the time to “act more as a guide for patients and spend the time to educate them, and help them make lifestyle changes that affect their health.” Ultimately, we learn, that clinic, too, has come under serious pressure to increase productivity. Dr. Martin is not covering her costs, and diminishing reimbursements are seen as a significant threat to the clinic’s viability. Dejected, she finds herself back where she started.
Also woven into the film’s fabric are other poignant stories from both the physician and patient side. We learn of military applications of acupuncture for pain relief, the film-makers document skeptical battle-hardened veterans as they find their way to “weird” but effective alternatives after conventional polypharmacy has failed them.
We follow the progress of Sgt. Robert Yates, a US Army infantryman and wheelchair-bound self-proclaimed “redneck,” who embarks on a quest to wean himself from a regimen of 32 drugs prescribed for his severe combat injuries and PTSD. Over a period of months, his health—and his outlook—are completely turned around thanks to an innovative Army program including yoga, meditation and acupuncture.
Narrow Strength, Broad Weakness
While acknowledging the strengths of American healthcare, Dr. Berwick shows also its unsatisfactory overall consequences. “If you need real serious technology today, like very complex cardiac surgery, you’re lucky to be in this country. Rescue care is second to none. But as an overall system, we’re not anywhere near the best in the world…Our lifespan isn’t even in the top twenty.”
Profit-driven healthcare, as opposed to patient-outcome driven healthcare, takes a beating from a variety of critics in Escape Fire. Physician-luminaries offering analyses include Cleveland Clinic chairman of cardiovascular medicine, Steve Nissen, MD, University of Arizona’s Andrew Weil, MD, and Dean Ornish, MD, whose pioneering research first showed that combinations of lifestyle change, meditation, exercise and psychosocial support could quickly reverse coronary artery narrowing.
Doctors emerge, not as “evil-doers” but as victims of a system that leaves them few options. Dr. Nissen: “Physicians are well-intentioned. Even when bad things happen, it’s not because people have bad intentions. It’s that our system is all fouled up.” He does go on to say, “When medicine became a business, we lost our moral compass and I think we’ve gotten into a great deal of trouble because of that.” He added, “What I’m arguing for is not to make things tough on industry, it’s to make things safe for patients, putting patients first.”
Dr. Weil points out, “A great deal of what’s done in conventional medicine is to put band-aids on things or to suppress symptoms.” After noting that profit-driven pressures have shrunk the time allowed for patient visits to 7 minutes with a patient, he warns that the “two-minute visit” is being discussed seriously. “Literally 30 patients an hour…And this is not the choice of the doctor,” he said.
Such a system, said Shannon Brownlee, medical journalist and author of Overtreated: Why Too Much Medicine is Making Us Sicker and Poorer, is really a “disease care system” that “doesn’t want you to die and doesn’t want you to get well – it just wants you to keep coming back for care of your chronic disease.”
Massive Re-Think
We hear from Wendell Potter, former director of Communications for CIGNA, who after a crisis of conscience left the insurance industry to speak against its practices (read HPC’s in-depth interview with Wendell Potter).
Steve Burd, CEO and president of the Safeway grocery chain outlines the company’s program to incentivize weight loss, smoking cessation and exercise for 30,000 Safeway workers, a program that has kept the company’s healthcare costs flat while the national average between 2005-2009 rose 40%. “Safeway employees will be less of a burden on Medicare of the future because we have adapted to this culture of health and fitness. You allow and encourage your employees to become healthier, they become more productive, your company becomes more competitive…Making money and doing good in the world are not mutually exclusive.”
Dr. Nissen’s Cleveland Clinic was founded by four physicians who realized they did better as a team than as individual practitioners. They formed a group practice and decided they would pay themselves a salary and that the money left over would go into growing the organization. That model has continued to this day. “We’re all salaried. So the decision on what we do for a patient is dependent upon what the patient needs, not on our financial incentives.”
“Achieving real solutions,” said Andrew Weil, will call for a “massive rethinking about healthcare at all levels of society…a huge effort.”
Escape Fire also spotlights Dr. Ornish’s decades of work to provide the hard science verifying the ability of non-pharmaceutical, non-surgical approaches to impact atherosclerosis and prostate cancer, even to influence gene expression, and teleromerase and teleromere length. “People often think it has to be a new drug or a new laser or something really high tech and expensive to be powerful, and they have a hard time believing that these simple choices that we make in our lives each day can make such a powerful difference,” Dr. Ornish said.
As Dr. Ornish—and the film viewers find out—the data were not the game-changer he’d hoped they would be. Data alone is seldom strong enough to dislodge entrenched behaviors, especially when the data fly in the face of their closely held beliefs and habits of thinking. It took a more fundamental understanding–that without reimbursement, the Ornish program, whatever its potential benefits would remain on the fringes of American medicine.
It took 16 years of persistence to wrest the power of the purse from a variety of insurers. In January 2011, Medicare finally agreed to reimburse physicians for implementation of the Ornish program for CVD reversal.
Escape Fire Premieres
In an interview conducted after a New York City screening of Escape Fire, Dr. Ornish commented that procedure-based reimbursement patterns are now shifting towards more diagnosis-based ones, such that a patient with a diagnosis of coronary heart disease will get a set amount of dollars for care. “So the kinds of things that we are doing, ultimately will be not just the right thing to do, but also a much more financially viable and sustainable way to practice.”
Cardiac surgeon Mehmet Oz, MD, director of the Cardiovascular Institute and Complementary Medicine Program at New York-Presbyterian Hospital, and host of the wildly popular “Dr. Oz Show,” acknowledged that excessive cardiac treatment occurs even though “sometimes there’s a simpler way to provide a more comprehensive solution to what patients need.” In remarks following the film, Dr. Oz commented that while changing the incentives in healthcare may help the situation, physicians, themselves, must make changes.
“Part of it is professionalism. Professionals police each other… If you’re clever enough to become a specialist in cardiovascular services, you ought to be clever enough to realize that bettering the field of medicine is part of our covenant.”
END
Author: Walter Alexander
Issue: Winter 2008: Cognition, Heart & Mind – Issue #54, Vol. 13
Study of Mistletoe Treatment for Colorectal Cancer
Among cancer patients being treated surgically for stage I-III non-metastatic colorectal carcinoma, those who received supportive care with the fermented mistletoe extract Iscador (ISC) (from Viscum album L.) along with conventional adjuvant (given after surgery) chemo- and/or radiotherapy had fewer adverse drug reactions (ADRs) as compared with those who received similar treatment with only passive aftercare. “Stage I-III” implies a range from very early stages to those in which the tumor has spread to nearby lymph nodes. The observational study was based on medical records from 804 consecutive patients (429 ISC, 375 controls) treated at 26 centers in Germany and Switzerland. The lead investigator was W.E. Friedel, MD, Hospital Bad Bocklet, Bad Bocklet, Germany.
Patients received subcutaneous ISC injections two or three times per week as part of long-term supportive care. Investigators compared ADRs related to conventional supportive care or to care with ISC added, duration of hospitalization, and disease-free survival (DFS). In their analysis, they adjusted for any differences in patients’ baseline characteristics that could affect outcomes.
After treatment of about two months and at a mean follow-up of 55 months, ADRs were reported in 19.1% of patients receiving ISC and in 48.3% of patients receiving passive supportive care. The difference was highly significant statistically. Side effects related to the gastrointestinal system and to the central nervous system, especially, were reduced among those receiving ISC. Karnofsky Index, a measure of a patient’s general status, which was actually lower (worse) at baseline in the ISC group, improved continuously in the ISC group and was still at baseline level in the control group at the end of therapy. Hospital stays were significantly shorter (mean 35.5 days ISC, versus 41.2 days in controls) and the hazard ratio (risk of experiencing a tumor-related event such as tumor recurrence, distant metastasis or death) was a significant 32% lower for the ISC group.
Systemic reactions caused interruption of therapy in 1.2% of cases and 23.3% of ISC patients had mild to moderate injection site reactions. No life-threatening or persisting ADRs were attributed to ISC, however, nor were any tumor increases reported with ISC.
Dr. Friedel concluded that in this largest-to-date systematic comparative clinical data evaluation concerning supportive mistletoe treatment in colorectal cancer, in the ISC group there were significantly fewer ADRs from chemotherapy/radiotherapy, fewer disease- and therapy-related symptoms, and longer disease-free survival. “Based on these data,” he said, “a prospective randomized clinical trial to confirm these results is warranted.”
Mistletoe for Pancreatic Cancer Treatment
In a further study of Iscador (ISC) as part of supportive care, the mistletoe extract demonstrated strong benefits as compared with conventional supportive care among patients with pancreatic carcinoma receiving adjuvant chemotherapy (with or without radiotherapy). “Adjuvant” signifies treatment given in addition to primary treatment (usually surgery). Chemotherapy among 400 patients treated at 17 German and Swiss centers was mostly gemcitabine.
Study author P. Heusser, MD, Institute of Complementary Medicine (KIKOM), University of Bern, Bern, Switzerland, noted that mistletoe therapy is often used in Europe as supportive treatment among cancer patients, mainly to reduce adverse drug reactions (ADRs) of conventional chemo- and/or radiotherapy and to improve quality of life. Dr. Heusser’s study was designed to evaluate the effectiveness and safety of ISC given as a subcutaneous injection two or three times per week in 205 patients, at any stage of pancreatic carcinoma, receiving adjuvant chemotherapy and/or radiotherapy, or passive aftercare. A control group of 195 patients received conventional therapy only. The primary outcome measure was rate of ADRs. Results were adjusted to compensate for differences in baseline differences.
Patients in the ISC group had a significantly lower ADR rate than controls (13.7% versus 48.9%). Persistent therapy-related symptoms after the first therapy course, especially gastrointestinal symptoms, central nervous system (CNS) symptoms or back pain, were consistently better in the ISC group. Karnofsky index improved in the ISC group and deteriorated in the conventional treatment group, with a significant 4.5% difference (mean values 79.1% versus 74.7%). Mean hospitalization duration was shorter in the ISC group (39.5 days versus 53.6 days), and overall survival (mortality hazard ratio) was better in the ISC group (42% lower mortality risk than controls). The mortality benefit was more pronounced in those with metastatic disease.
Dr. Heusser underscored that this study is the largest systematic comparative clinical data evaluation ever performed concerning supportive mistletoe treatment in pancreatic carcinoma. Aside from the positive findings in reduced ADRs and symptoms, the longer overall survival suggests an independent beneficial effect in all pancreatic carcinoma tumor stages.
Author: Lilipoh editor Walter Alexander interviews Rollin McCraty, PhD, research director of the Institute of HeartMath
Issue: Spring 2009: Redefining Education – Issue #55, Vol. 14
 The Institute of HeartMath, founded in 1991 by Doc Childre, has conducted groundbreaking research on heart/brain communication and the power of coherence, a highly efficient psychological state where all the systems of the body work together in harmony. Out of that research have come scientifically validated stress relief products and services. After conducting the interview below, I asked for a review sample of one of the HeartMath stress monitoring devices. I was given a choice: either the hand-held emWave Portable Stress Reliever or the emWave Stress Relief System. I opted for the latter because of its PC full-screen readout. Not only does the software provide a real-time display of heart rate monitoring, it produces moving bar graphs of coherence, broken into low, medium and high coherence levels.
The Institute of HeartMath, founded in 1991 by Doc Childre, has conducted groundbreaking research on heart/brain communication and the power of coherence, a highly efficient psychological state where all the systems of the body work together in harmony. Out of that research have come scientifically validated stress relief products and services. After conducting the interview below, I asked for a review sample of one of the HeartMath stress monitoring devices. I was given a choice: either the hand-held emWave Portable Stress Reliever or the emWave Stress Relief System. I opted for the latter because of its PC full-screen readout. Not only does the software provide a real-time display of heart rate monitoring, it produces moving bar graphs of coherence, broken into low, medium and high coherence levels.
At home, I loaded the software and hooked up the USB finger cuff and tried it out. What was initially shocking was that although with relative ease and modest concentration I could get myself calm with a heart rate in the upper 50s (bpm), the bar charts showed my “coherence” levels to be in the basement 100% of the time. Only during listening to some “serious” music did I see the middle coherence bar move up, and then working intensively with some meditative verses I graduated to a few stretches with more than 50% of the time in the middle and high coherence realms. I was still at the lowest challenge level.
A few days before this writing, it was announced that the portable device won the Last Gadget Standing People’s Choice Competition at this year’s Consumer Electronic Show. The HeartMath Institute offices and laboratory are nestled deep in a Redwood forest near Boulder Creek, California, at the end of a series of switchbacks more than an hour south of San Francisco. There I interviewed research director and co-founder Rollin McCraty.
LILIPOH: Let’s start with the name—HeartMath. Why?
Rollin McCraty: When I met Doc Childre 23 years ago, he showed me what he had found—that the heart is the access point to the higher part of ourselves. He saw also that our planet was going into a rapid shift—which we are in now. A shift that creates a lot of stress—stress necessary for that transition. That’s what the HeartMath tools are about—to help people with that stress and to understand that the transition is from mind-based awareness to heart-based awareness. This isn’t a metaphor. It’s literal. The idea is to help people ease through that transition.
L: So you teamed up with him?
RM: I walked away from a multimillion-dollar company that I owned to join him with the other co-founders to help people move more toward the heart.
L: So the name—to balance what we used to associate with “heart?” When my brother and I would buy frilly Hallmark cards with hearts on Mother’s Day for Mom.
RM: And to get it away from Valentine’s Day sentimentality, too.
L: That’s related to why Rudolf Steiner insisted on the term “spiritual science”—and then there’s the science, itself, of course. I see you have your laboratory in this building. Can you share some of the key insights that have come out of your work here?
RM: Actually, some of the key knowledge predates our work by a hundred years. About 90 percent of the fibers among the 3000+ in the parasympathetic nervous system’s vagus nerve are afferent, ascending. They are monitoring the body and sending information to the brain. And only ten percent go the other way from the brain to the body.
I doubt that more than a few physicians know this, but in reality, neurally speaking, the heart sends far more information to the brain than the brain sends to the heart. No other part of the body has that level of afferent connection to the brain. Other research carries this farther, and shows that it is the heart that modulates brain function and perception.
L: Which speaks to the heart’s primacy as a sense organ, rather than as a pump.
RM: Yes. A hormonal gland and a sensory organ with forty thousand sensory neurons. And not just sensing the body. In our electrophysiological work—it’s surprisingly easy to do these studies with signal averaging techniques—we can quite literally measure my heartbeat in relation to your brain waves at conversational distances. Information is being transferred at an energetic level. With an instrument, a $40,000 magnetometer, we can detect the magnetic field of the heart at about three feet from the person, and the brain at about three inches. But we can measure the effects between people at much greater differences by monitoring their EEGs and ECGs.
L: Which is to say that the nervous system is much more sensitive than the $40K device.
RM: And that our connectedness is measurable at a physiological level. Not only can I detect your heartbeat in my brain waves, but especially if I’m in a deeper coherent state, my brain waves will synchronize to your heartbeat—measurably. And it goes way beyond that.
Winfried Otto Schumann (1888-1974) predicted resonant frequencies in layers of the ionosphere that have since been verified. It turns out that some of these frequencies are in the same range as those of human brain and heart activity. You can think of them as the brain waves and heart rhythms of the planet, and there is an amazing overlap with human biological rhythms.
L: How does that manifest in actual events?
RM: Some large-scale studies in the US and in Russia have shown that when you have disturbances in the geomagnetics of the earth (which are related to high solar activity), the incidence of heart attacks goes up—along with traffic accidents, suicides, rates of depression. Even PSI abilities are modulated by these rhythms.
L: Can you say more about the connection to health?
RM: Franz Halberg, the founder of chronobiology, found that of all the bodily systems, the most reflective of changes in geomagnetic activity is the human heart. And the best measure of that is heart rate variability or HRV, which is a measure of beat-to-beat changes in both the strength and duration of the heartbeat. It has been very well established that low HRV is a strong predictor of future health problems—including all-cause mortality. It’s a better predictor of future mortality and morbidity than any of the standard risk factors—like cholesterol levels or smoking. HRV has been one of our primary fields of research since before it was considered important among conventional clinicians.
L: Why is too little HRV a negative predictor?
RM: Age is the strongest factor, with younger people having greater HRV—and it diminishes as we age. But there are examples of older people with very high HRV—and they are invariably very healthy, vibrant individuals. I have come to view HRV as a measure of vitality, of the integrated wholeness of a person. Low HRV suggests depletion and psychological rigidity.
L: I’ve heard at cardiology conferences that low HRV predicts future heart attacks.
RM: Stewart Wolf showed back in the ‘60s that those whose HRV did not return in the first weeks after a heart attack were less likely to survive–but it took him 10 years to get it published. Now there are more than two-hundred thousand papers on the subject.
L: What factors besides age negatively impact HRV?
RM: It’s very clear now that if you have accumulated emotional stress, depression, anxiety or prolonged physiologic stress—at an emotional level, that accumulated stress results in reduced HRV. We’re involved with a few Olympic teams where we are using HRV to test for overtraining. When you start depleting the system rather than replenishing, it shows up—HRV is a very sensitive indicator. I don’t know of a better physiological measure that really gives us a measure of overall . . . what I like to call integrated energetic physiologic vitality.
L: And here’s a chance to make the connection with your commercial products.
RM: That’s our stress research. Certain emotions and attitudes deplete our energy reserves, while others renew them. It really gets down to being that simple—learning to have more self-regulation and choice in our emotional diet.
The scientific community has not done humanity justice, regarding emotion. It’s still not understood. Recent books are still saying that emotions are something that happens to us and we have no control over them. That’s utter nonsense.
L: It’s the transformation that our time is about.
RM: Yes. From brain-based to heart-based. And that brings in another variable, beyond the quantitative HRV measure—which is pattern. If you look at these two heart rhythms (see figure), the amplitude is exactly the same between two decimal points, but even so, they are profoundly different. In the top one there’s a desynchronization of the two branches of the autonomic nervous system.
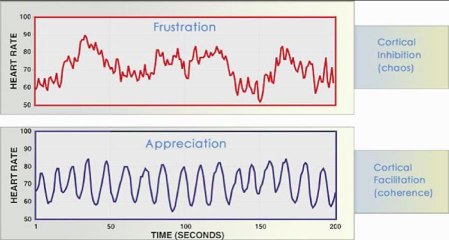
Literally, it’s like driving your car with one foot on the brake and one on the accelerator at the same time. What are we doing then? We’re burning a lot more gas, depleting the system, putting more stress and wear and tear on it—and the heart has a jerky ride. This is a rhythm now associated with what’s being called cortical inhibition—termed that by a famous husband and wife team, the Laceys, in the ‘70s. They got the paradigm to start to shift away from the notion that everything is being controlled from the brain, and moved things back towards the body and heart. The bottom rhythm is the one the system naturally goes into when we’re feeling emotions of appreciation, care, love, compassion or gratitude—and it facilitates cortical function. The chaotic rhythm is associated with cortical inhibition.
L: And the HeartMath products?
RM: They are simple tools to help us learn to catch those chaotic emotional waves and then manage and transform them into coherence.
L: You mentioned coherence before. Please say something more about what you mean by it.
RM: Technically, coherence is the harmonious flow of information, cooperation, and order among the subsystems of a larger system that allows for the emergence of more complex functions. It brings with it more ordered mental and emotional processes as well as more ordered and harmonious interactions among various physiological systems. It’s a dynamically stable state, out of which sensitivity to another level of information arises. Speaking philosophically, coherence increases our contact with our higher self. It expands our access to higher consciousness tools—and it’s really about the shift we are going through from the mind to the heart. It’s another dimension of intelligence that makes life easier.
L: How easier?
RM: We can learn rhythm through resistance.
L: Please explain rhythm and resistance a bit more.
RM: Resistance refers to both the external sources of stress that we encounter in day-to-day life and our own internal resistances to self-regulation, our changing moods, and so on. As we learn to find the flow or coherence, we often find that we can find a balanced rhythm to help navigate the resistances with more ease and grace. It is knowing when to push through, or back off for a while, etc. Learning to follow the heart’s intuition is often one of the most effective ways to find this rhythm and balance.
L: Can we go back to this resonance between the individual or groups of individuals and the ionosphere? I first learned about your work through James Dyson (see LILIPOH, Issue 54, Winter 2008). And he mentioned that connection as being reciprocal—which is consistent with what I am familiar with from Steiner—but still shocking.
RM: For most people it is not too far of a jump to accept that we are born into and live in the earth’s magnetic field. We go a step further in our hypothesis—check out the Global Coherence Initiative on the web—positing that strong human emotions modulate the earth’s magnetic field. Not only can planetary stress waves be created, but you can also create planetary coherence waves. There’s some data to support that this may not be so far out.
L: For example?
RM: Two lines of evidence. There’s a long history of research showing that human emotion will cause otherwise random events to stop being random. Fifty years ago it was shown that nuclear decay can be modified by human emotion, and more recently studies have shown that strong emotion, especially collective strong emotion, makes random number generators stop being random.
Roger Nelson, retired from Princeton, set up a worldwide network of random number generators plugged into a central server. The number streams from those RNGs all went off randomness on 9/11 in the same way—and they did it 2-3 hours before the first attack. Such a planetary stress wave suggests collective intuition. Magnetic field detectors over the US east and west coasts also registered changes before, during and after 9/11.
We saw smaller RNG effects, but definite ones both locally and globally, during the millennium year celebrations. We watched the effect, about a quarter of the way out of randomness, march right around the planet.
L: This helps us go from the wonderful sentiment “we are the world” toward an understanding that it’s not just a sentiment, but actually fact. What really becomes almost absurd, then, is that we are fallen into a state that assumes we are not connected to the rest of creation. But there are reasons for that, too. So how do you gather more proof of this sort, and then what do you do with it?
RM: That’s the Global Coherence Initiative.* You organize large groups of people who’ve learned how to achieve coherence. You get them to report their coherence data back to you while you simultaneously monitor the earth’s rhythms. It will take years to really test this thoroughly, but we will be measuring a large number of humans in a coherent state with a shared positive intention—powered by emotions of care and compassion, that’s the key—not thought—while we simultaneously monitor the earth’s fields, and another social outcome variable, hopefully.
L: You know—you’d probably agree with me if we talked this out—the notion that you can have compassion or caring without a thought content is not a true one. Georg Kühlewind coined the term “cognitive feeling”—with regard to feeling states that are not subjective, but that actually convey knowledge or understanding. Also, you have to have compassion towards someone or something, or gratitude or appreciation for something. I presume you’re targeting cold abstract thought, the monkey mind, as a negative, and not living thought in the realm of meaning.
RM: I can agree with that. I think we think as we feel, not the other way around.
L: And these coherent emotional states, of course, resonate between people.
RM: Between people, and between people and animals. We’ve shown both. I can show you EEGs of two people about five feet apart, where one person’s brain waves literally synchronize to another’s who is in a coherent state. I can also show you a person’s chaotic brain waves become coherent as she pets her dog. And there’s a dramatic shift in the dog, as well. It’s been shown with horses, too. I’m pretty convinced.
L: Something you’d expect, but it is good to see it. The relation to future events is much harder, isn’t it?
RM: We have shown that, too—following some of Dean Radin’s work at IONs** with people being shown randomly selected images, some of them really disturbing or violent images and some pleasing or beautiful. When someone is in a coherent state, the heart sends an afferent signal to the brain before the disturbing picture is shown. Certain specific brain signals have been understood to signify when one becomes conscious of something. In this test, they occurred a full second and a half after the heart knows, according to the potentials measured in the heart. We’ve published our data in a peer-reviewed journal (R. McCraty, M. Atkinson, R. T. Bradley – Journal of Alternative and Complementary Medicine 2004). What this is saying is that the heart appears to have access to a field of knowledge not limited by time and space.
L: So the challenge for us is to have access to what our hearts know.
RM: Yes. To me it is higher self, spirit, whatever term you put on it. It’s not a big jump to say we have this system and the heart is its central nodal point. It’s the primary conduit to the spirit part of ourselves—so that whenever we are in a coherent state and able to manage our emotions, especially positive emotions that amplify the force of intuitions, we facilitate the flow of information from the higher self, spirit, into the human mind/brain system. You could spend a lifetime studying HRV and the rhythm between heartbeats where the intuitions are encoded.
L: But the goal then would also be to apply them in practical ways. To adults, to children, even.
RM: Yes. My observation is that the heart rhythms of kids reflect much higher levels of coherence. I proposed a study with some graduate students to look at children up to about 5th grade to establish baseline levels of coherence. With that, we want to look at changes over time between different educational sytems—between urban, Seventh Day Adventist and Waldorf schools
Also, we have a program called HeartSmarts which aims at helping kids to stay inwardly connected. The most exciting part, to me, is that with it, a subset of high school kids were literally able to establish a new physiological baseline—one where coherence had become their new, established familiar state.
L: That is a great gift.
RM: In the military, our HeartMath devices are being used in about 35 VA hospitals. With reports coming out that they are the best thing yet for post-traumatic stress disorder and other reintegration issues for returning vets, they’re getting support from some high level generals.
L: I would think that these devices can help sidestep some of the stigma issues that many in the military have with going to a psychotherapist.
RM: Yes. Many have that. But, so many have reintegration issues. We’ve developed a phone coaching model for working with the emWave device.
L: You’re doing a lot of good work. How do you prioritize what to do first each day?
RM: Intuition. I make a list on the board and ask which makes most sense for me to do today?
L: Well—thanks ever so much!
* www.glcoherence.org
**Institute of Noetic Sciences